In early 2025, Alberta Health Services (AHS) commenced their Calgary Zone Green Team Competition in partnership with the Centre for Sustainable Healthcare, a clinical leadership and engagement programme for healthcare organisations wishing to improve the sustainability of their services.
This was our second competition with AHS, but CSH’s first ever licenced competition. After collaborating closely with us during the 2024 competition, Jelena Poprzen, Clinical Quality Improvement Consultant, took the lead in facilitating teams through this year’s event.
This marks a significant milestone for the Green Team Competition. Not only was the competition hosted by the organisation, but it was also led from within, showcasing AHS’s leadership in advancing sustainable healthcare improvement. By stepping into the facilitator role traditionally held by CSH, Jelena and AHS have demonstrated how this model can be effectively embedded at a local level, with clear potential for scaling and adaptation by organisations working in partnership with CSH—both across the UK and internationally.
Project support and implementation
Through the programme, five clinical teams across AHS were supported by Jelena Poprzen to add sustainable value within Green Team programme model and Sustainability in Quality Improvement (SusQI) methodology while carbon footprinting training and analysis were provided by CSH sustainability analysts.
SusQI is an approach to improving healthcare in a holistic way, by assessing quality & value through the lens of the sustainable value equation. The teams were encouraged to consider each element of sustainable value to identify high impact improvement ideas then plan, implement and measure the impact of their projects.


“’I appreciated the opportunity to contribute to meaningful initiatives that align with our values and make a real difference. It was energising to see how small ideas could grow into impactful solutions when supported by a motivated team and a shared purpose.”
Candice Horbay, Unit Manager AHS
Showcase Event
At the 24 September Showcase Event, five clinical teams from Alberta Health Services Calgary Zone presented their sustainability projects, outlining their achieved and anticipated savings, lessons learned, and opportunities to scale and spread.
Dr Colin Del Castilho MD, Associate Zone Medical Director Community, Rural and Continuing Care Facility Medical Director South Health Campus, stated that this was another excellent Green Team Competition hosted at the South Health Campus. The projects showcased this year built on the success of last year’s competition, highlighting a diverse range of innovative initiatives spanning inpatient units, operating theatres, and outpatient clinics.
The event was attended by colleagues and a judging panel including:
- Mark Anselmo, CZ Medical Director, AHS
- Harry Vandermeer, Executive Director, Office of Sustainability & Energy Management, AHS
- Shawna Syverson, CZ Chief Zone Officer, AHS
- Colin Del Castilho, SHC Facility Medical Director, CZ Associate Zone Medical Director, AHS
- Rachel McLean, SusQI Programme Lead, Competitions and Specialty Challenges, Centre for Sustainable Healthcare, UK

“The five teams that presented their high-impact sustainable projects utilising the Sustainability in Quality Improvement (SusQI) methodology were incredibly remarkable. Each of the projects yielded high environmentally friendly results, as well as patient, physician, and staff experience improvements. The projects all had low costs to implement and significant cost savings. This work should be a priority to spread across all of Alberta Health Services.”
Shawna Syverson, Chief Zone Officer. Calgary Zone
What makes this work particularly exciting is its potential for large-scale adoption and spread across Alberta Health Services.
The impact
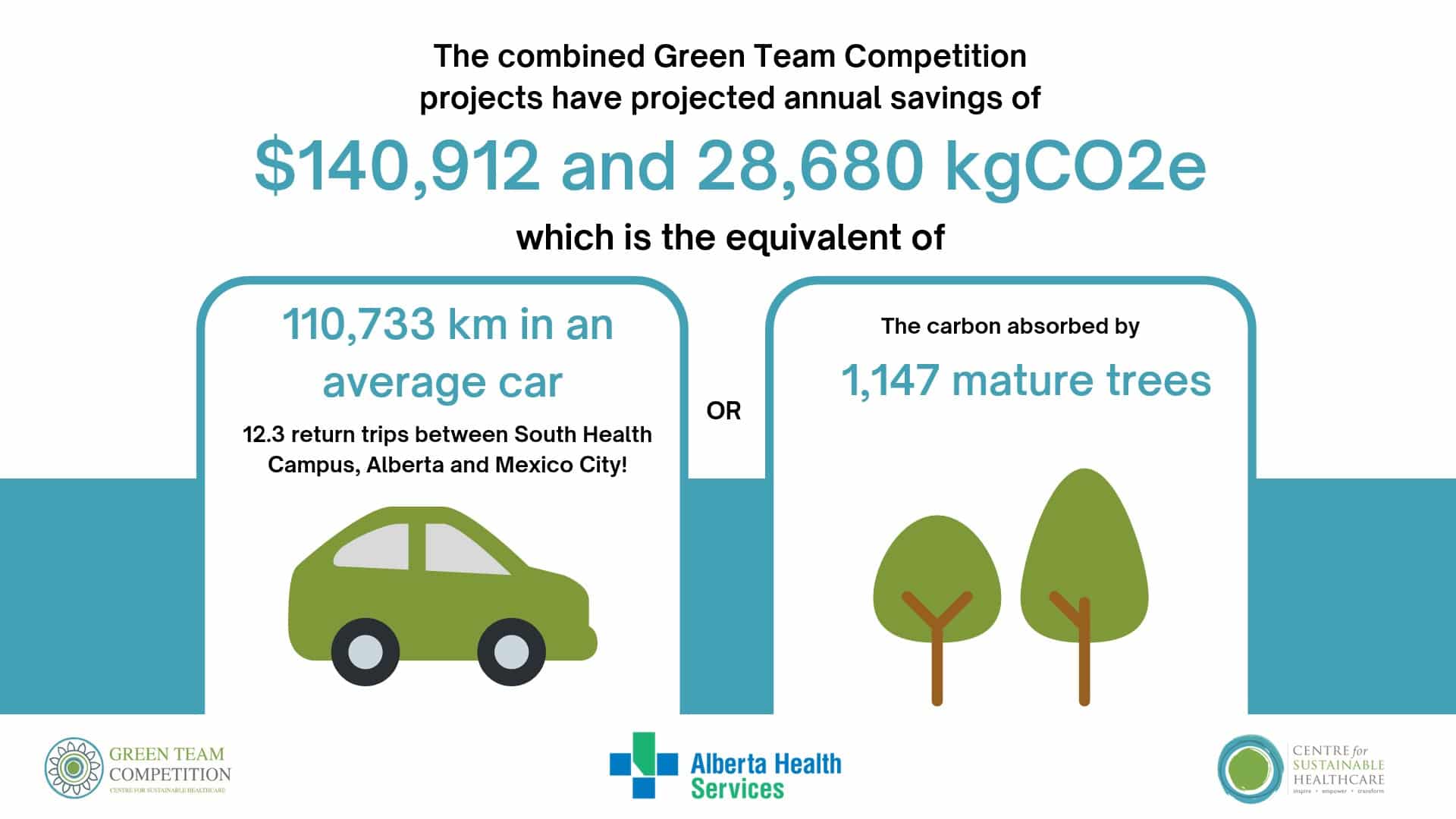
The Green Team Competition has brought meaningful, measurable value to AHS. Collectively, the projects delivered through the competition are forecast to achieve $140,912 CAD in annual cost savings and cut carbon emissions by approximately 28,680 kgCO₂e each year.
That’s the environmental equivalent of:
- Driving more than 110,733 km in an average car
- Completing roughly 12.3 return journeys between South Health Campus in Alberta and Mexico City
- The annual carbon absorption of around 1,147 mature trees
More than just numbers, the programme has helped ignite a culture of sustainability across clinical teams, encouraging greener, smarter, and more person-focused ways of delivering care.
These early successes show the potential of grassroots, well-mentored initiatives to support the NHS’s net zero ambitions while improving patient outcomes and operational efficiency.
Winners
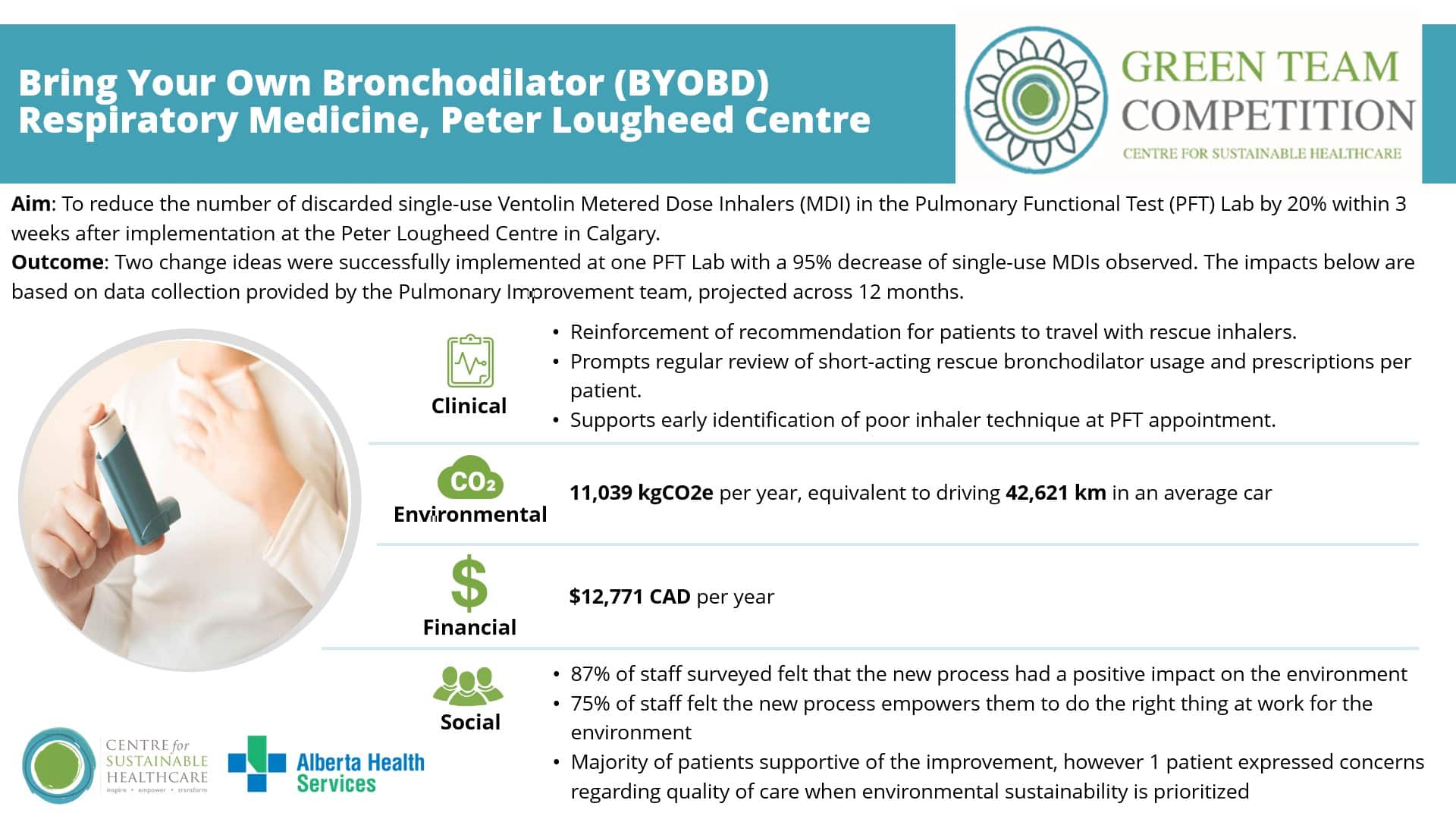
Congratulations to the winning team behind the Bring Your Own Bronchodilator (BYOBD) project.
Their innovative initiative tackled the significant waste generated from single-use Ventolin inhalers in pulmonary function testing by introducing two key changes: enabling patients to use their own prescribed inhalers and implementing a safe multi-patient use protocol. The project achieved impressive reductions in carbon emissions and cost, while maintaining patient safety and enhancing staff engagement in sustainable practice.
This project exemplifies how clinical innovation and sustainability can go hand in hand, setting a strong precedent for scalable, evidence-based change across Alberta Health Services and beyond.

“An amazing experience — with support from the Department of Medicine Planetary Health team, the CSH SusQi Green Team, PLC and Pulmonary leadership, our team achieved impressive cost savings and a significant reduction in carbon footprint within just 12 weeks.”
Dina Fisher MSc MD FRCPC, Site Lead – Pulmonary Medicine Peter Lougheed Center Division of Respiratory Medicine University of Calgary
Highly Commended
Congratulations to the COVID-19 Cycle Threshold (Ct) Value Project Team, recognised for their forward-thinking approach to integrating laboratory data into clinical decision-making.
Their project applied real-time Ct values to guide safe and earlier discontinuation of isolation precautions for immunocompetent patients with COVID-19, reducing unnecessary PPE use, freeing isolation rooms, and improving patient flow—all while maintaining high standards of care and infection prevention.
The judges commended this project for its interdisciplinary collaboration, data-driven approach, and clear potential for system-wide adoption. It demonstrates how thoughtful innovation can simultaneously improve patient experience, operational efficiency, and environmental performance.

“Participating in this competition provided a valuable opportunity to demonstrate the potential impact of our ideas on both environmental outcomes and broader systemic changes. We are excited to continue refining out approach and monitoring real-time results in the coming months.”
Alaina Bosinski R.N B.N Manager, Foothills Medical Centre Team
The Centre for Sustainable Healthcare would like to thank and congratulate all teams that took part in the competition. The outcomes of the competition stand as a testament to the dedication and innovation of each team in advancing the sustainability of healthcare at AHS.
Green Team Competition projects
Read the full Impact Report here or view the project summaries below.
1. BYOBD – Reducing single-use metered-dose inhaler use in the pulmonary function lab, Peter Lougheed Centre Team
Team members:
- Dina Fisher – Respiratory Physician Lead PLC
- Joel Chen – Respiratory Physician PLC
- Dawn Papp – PLC Respiratory Services, Pulmonary Diagnostics Supervisor
- Alan Sutton – PLC Respiratory Services, Pulmonary Diagnostics Manager
- Claire Barber – Associate Vice Chair Planetary Health DOM
- Arooj Nazir – Quality & Process Improvement Consultant
- Kiran Dhiman – Research Coordinator & Precision Health Student in Quality Improvement and Safety Health Leadership
- QI Group: Jelena Poprzen, Monica Veness – Clinical Quality Improvement Consultants
- Omenaa Boakye – Lead, Provincial Projects-Acute Care Alberta
Setting / patient group: Outpatient pulmonary function testing (PFT) lab.
Summary
The team identified that single-use Ventolin metered dose inhalers (MDIs) were being used for each patient during bronchodilator responsiveness testing in pulmonary function testing (PFT) labs, with approximately 98% of the medication remaining unused. To address this, they introduced two interventions: allowing patients to use their own prescribed inhalers and implementing a protocol for safe multi-patient use of Ventolin MDIs. These changes were supported by staff education, stakeholder engagement, and updated infection control guidance.
Outcomes
The initiative reduced MDI waste from 23 to 1.25 inhalers per week at the Peter Lougheed Centre PFT lab, saving an estimated 11,039 kgCO₂e annually—equivalent to driving 2,859 km in an average car—and $12,771 CAD per year. Expansion across all four acute care sites in the Calgary Zone could save 44,154 kgCO₂e and $51,086 CAD annually. Staff reported feeling empowered to make sustainable changes, and patient safety and clinical standards were maintained.
2. Use of Serial Cycle Threshold Values for SARS-CoV-2 to Assist Early De-Isolation of COVID-19 Positive Patients on a Medical/Surgical unit, Foothills Medical Centre Team
Team members:
- Alaina Bosinski (Patient Care Manager)
- Candice Horbay (Unit Manager)
- Amber Martin (Clinical Nurse Educator)
- Dr Heidi O’Grady (Infection Control Professional)
- Dr John Conly (Infectious Diseases Physician)
- Nikita Baker (Quality Improvement Consultant)
- Sheena Hammond (Quality Improvement Consultant)
- Kevin Huntley (Pulmonary Nurse Practitioner)
- Mohamad Hlaihel (Nurse Clinician)
- Kathleen Lowe (Nurse Clinician)
- Pamela Schmidt (Nurse Clinician)
- Dr Byron Berenger (Medical Microbiologist and Provincial Microbiology Section Chief, APL)
- Dr Chris Hergott (Respiratory Medicine Site Lead)
- Rachel Rouble (Executive Director)
Setting / patient group:Acute care hospital – Primary respirology unit, immunocompetent COVID-19 management
Summary
The team identified that current guidance for managing immunocompetent COVID-19 positive patients required contact and droplet precautions for 11 days, regardless of symptoms. This led to extended isolation periods, increased PPE use, and strain on patient care and resources. To address this, the team developed a new process using real-time cycle threshold (Ct) values from PCR tests—alongside clinical assessment—to determine when isolation could safely be discontinued. Nurse Clinicians and Infection Prevention and Control teams conducted daily reviews, supported by education materials and a shared tracker to guide consistent decision-making.
Outcomes
Modelling from the previous year suggested that 56.6% of admitted patients would qualify for early de-isolation, reducing isolation by an average of 3.09 days per patient. Projected annual savings include 12,522 kgCO₂e and $77,607 CAD, achieved through reduced PPE use and improved resource efficiency. Staff reported fewer care delays and improved workflow, while patients experienced enhanced care access and reduced distress associated with prolonged isolation. This initiative demonstrates how Ct-informed decision-making can improve care quality, reduce waste, and strengthen system sustainability across Alberta Health Services.

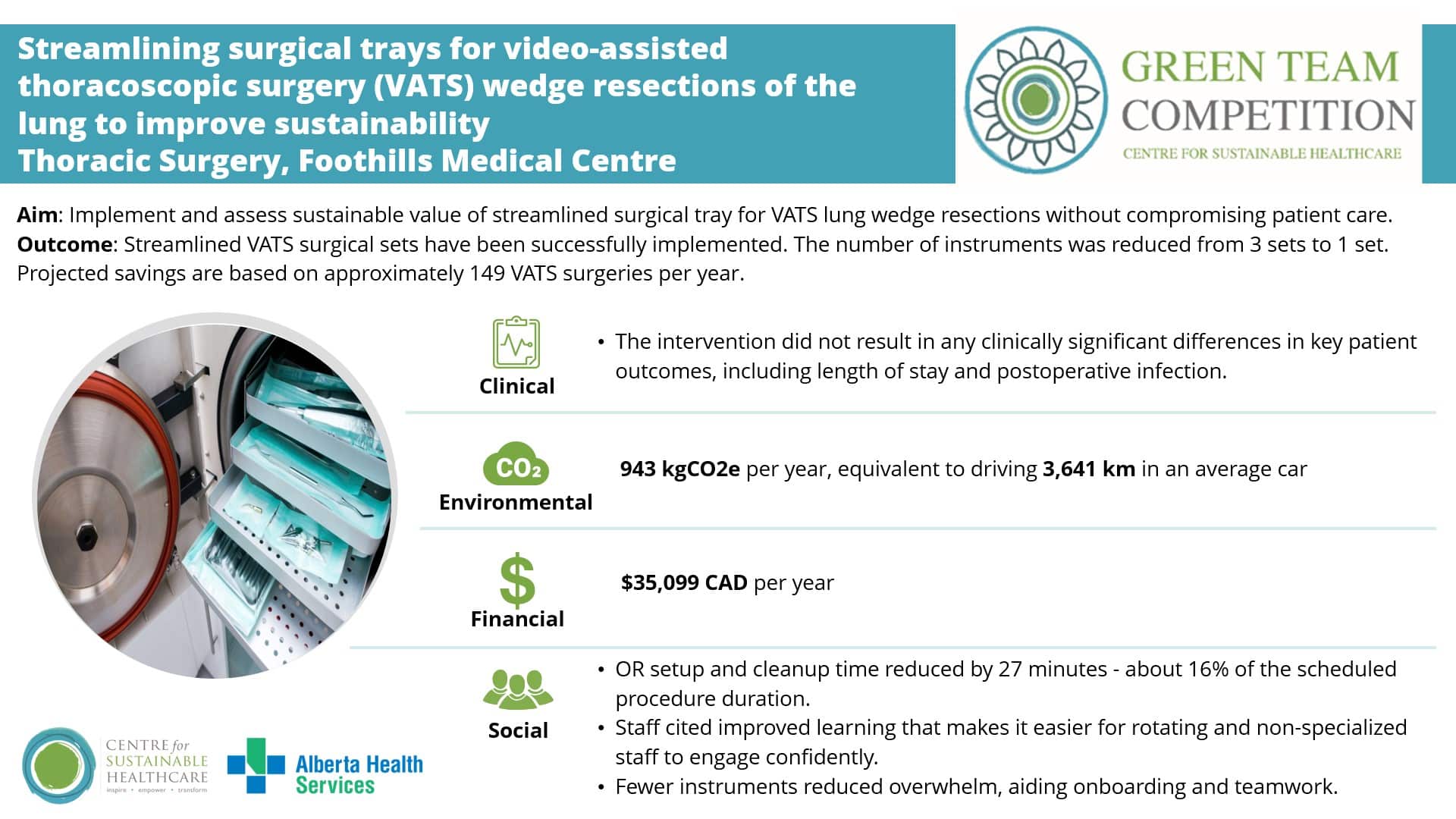
3. Streamlining surgical trays for video-assisted thoracoscopic surgery (VATS) wedge resections of the lung to improve sustainability, Thoracic Surgery Team Foothills Medical Centre
Team members:
- Andrew Graham (Thoracic Surgeon)
- Rajajee Selvam (Thoracic Surgery Fellow)
- Megan Muir (OR Nurse Clinician)
- Hector Gomez (MDRD Manager)
- Jennifer Bolt (Analyst)
- Francisco Aguirre (QI Consultant)
- Crispin Russell (Thoracic Surgeon)
Setting / patient group: Video-assisted thoracoscopic surgery (VATS) lung wedge resection procedures.
Summary
The team identified that VATS lung wedge resections were being performed using the same full surgical tray as more complex procedures such as lobectomies, resulting in numerous unused instruments, excess reprocessing, and unnecessary waste. To address this, they designed and implemented a streamlined surgical tray tailored to wedge resections. The intervention involved an audit of instrument use across 17 cases, staff surveys, and a multidisciplinary focus group to refine the tray design. Supported by operational leaders, the new tray was tested using a Plan–Do–Study–Act (PDSA) cycle from March to May 2025.
Outcomes
Patient outcomes remained stable, with the median length of stay reduced from 1.41 to 1.21 days, and no increase in complications. Efficiency improved, with OR setup and cleanup time reduced by 27 minutes per case. Consumables were cut from 24 to 8 per procedure, and MDRD sets reduced from three to one, resulting in an estimated annual saving of 946 kgCO₂e—equivalent to driving 3,641 km in an average car—and $35,099 CAD in cost savings. Staff reported greater procedural efficiency, improved learning opportunities, and strong support for reducing healthcare’s environmental impact. The project demonstrates how a collaborative, multidisciplinary approach can deliver measurable environmental, financial, and workflow benefits while maintaining high-quality patient care.
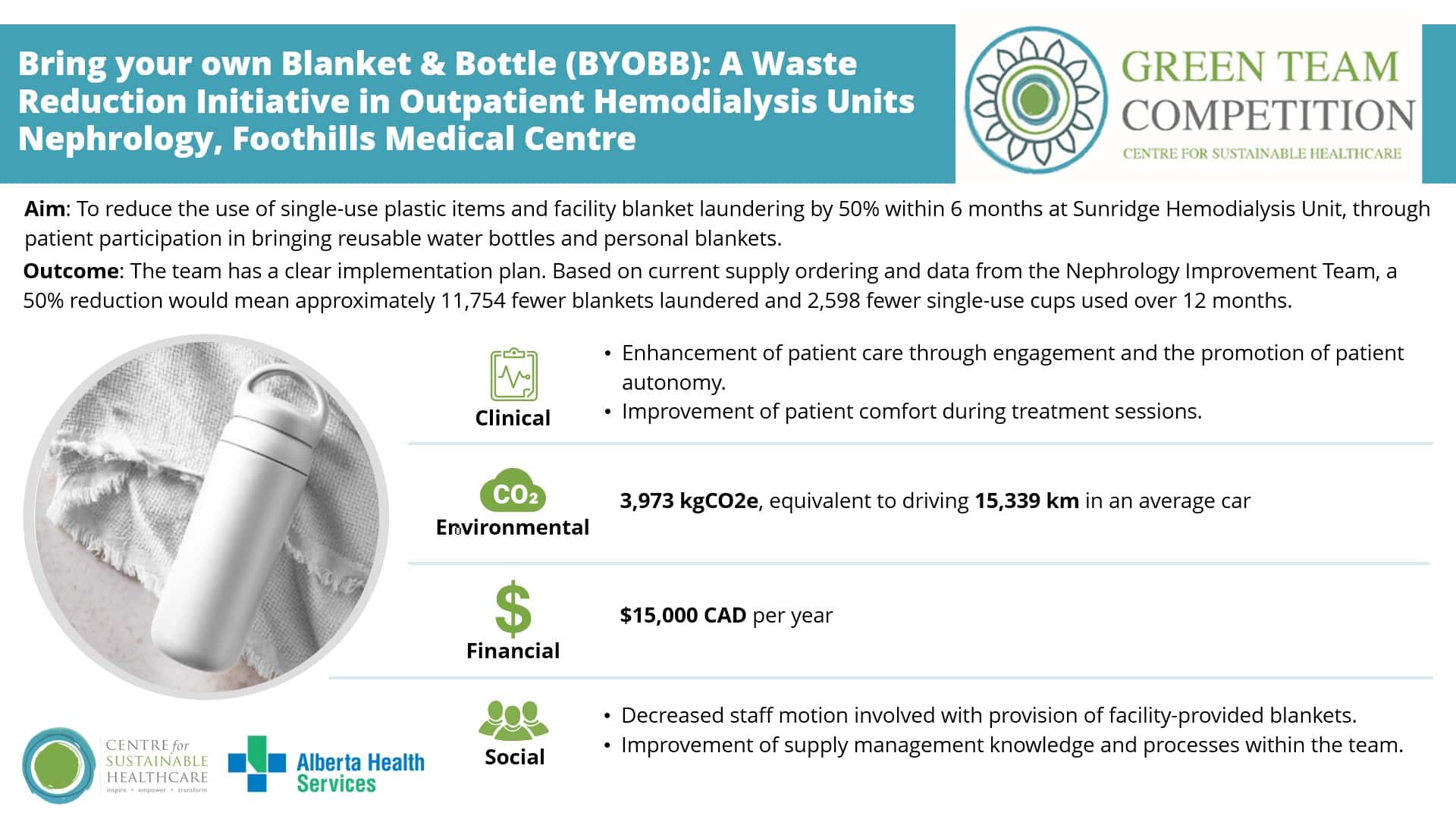
4. Bring your own Blanket & Bottle (BYOBB): A Waste Reduction Initiative in Outpatient Hemodialysis Units, Nephrology Team Foothills Medical Centre
Team members:
- Dr. Bhavneet Kahlon – Nephrologist (bhavneet.kahlon@ahs.ca)
- Arooj Nazir – Quality & Process Improvement Consultant (arooj.nazir@ahs.ca)
- Jelena Poprzen – Clinical Quality Improvement Consultant
- Monica Veness – Clinical Quality Improvement Consultant
- Claire Barber – Associate Vice Chair Planetary Health for the Department of Medicine
- Kiran Dhiman – Research Coordinator & Precision Health Student
- Anuk Ghimire – Nephrologist
Setting / patient group: Patients receiving hemodialysis in a Canadian Hospital.
Summary
The team identified that outpatient haemodialysis (HD) units produce large amounts of waste and emissions due to heavy reliance on single-use items such as plastic cups, lids, and spoons, and from laundering hospital-provided blankets. To address this, the Bring Your Own Bottle and Blanket (BYOBB) initiative was launched at Sunridge Haemodialysis Unit, encouraging patients to bring reusable water bottles and personal blankets. Supported by Infection Prevention and Control, Supply Management, and Environmental Services, the project included process mapping, baseline data collection, and equity considerations to ensure participation remained voluntary and patient comfort was not compromised.
Outcomes
Modelling based on current supply data suggests that a 50% reduction in blanket laundering and single-use plastics would save approximately 3,972.7 kgCO₂e annually—equivalent to driving 15,339 km in an average car—and $15,000 CADper year. The initiative is expected to improve patient experience, reduce staff workload associated with blanket provision, and enhance understanding of supply processes. Despite operational and logistical challenges, early engagement with infection control and environmental services established a strong foundation for safe, scalable implementation across other outpatient HD units.
5. Encouraging slow IV push of antibiotics (tazocin, teicoplanin, ceftriazone) instead of saline bag administration, Emergency Department (ED) Nursing Team
Team members:
- Stephen Caron – Patient Care Manager – PLC Women’s Health
- Katey Cha – Unit Manager (interim) – PLC Day Surgery and Surgical Short Stay
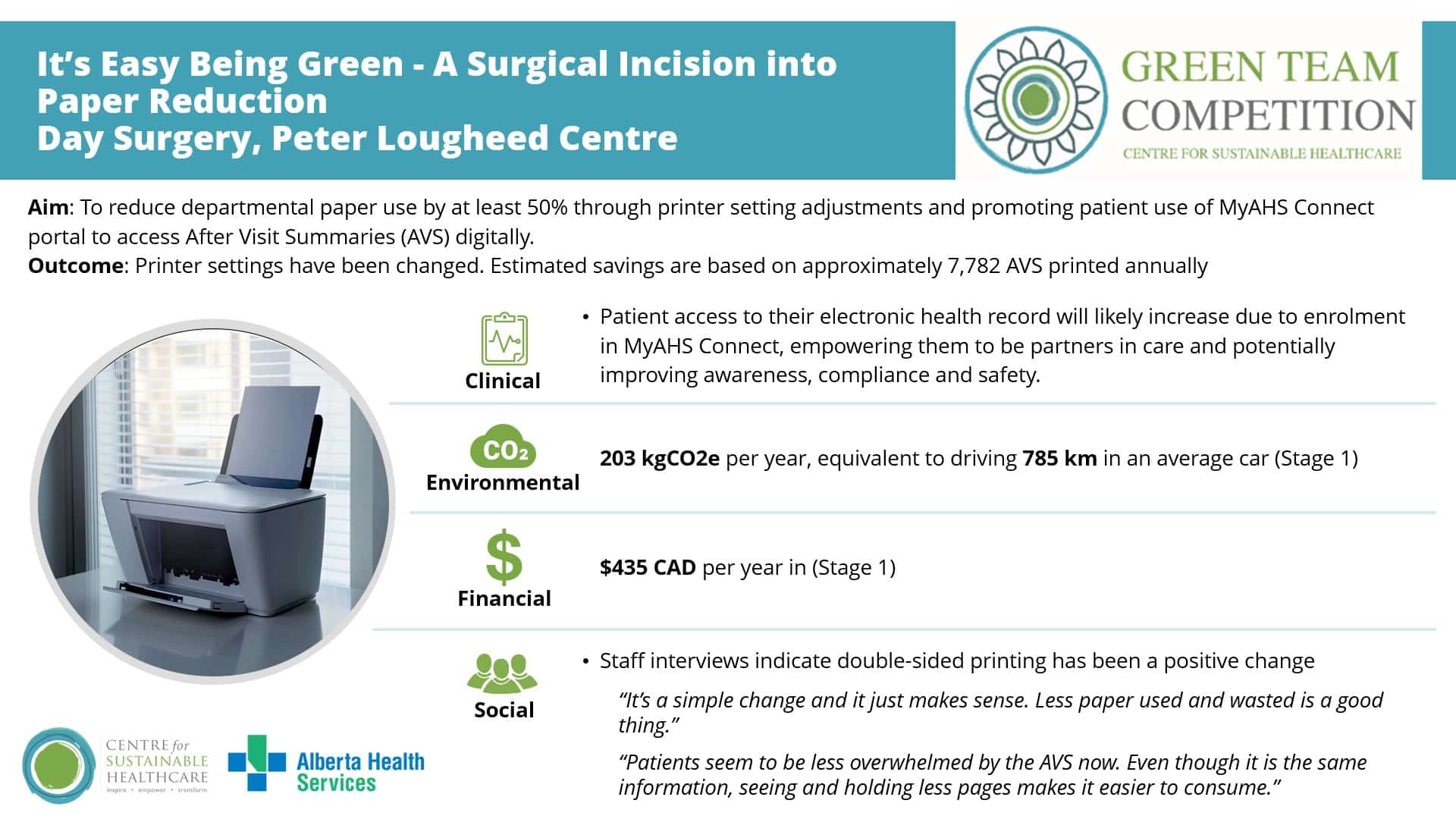
Setting / patient group: Day surgery department.
Summary
The team identified a long-standing reliance on 100 ml saline bag infusions for administering IV antibiotics in the Emergency Department, contributing to excess plastic waste, higher costs and potential treatment delays. To address this, they launched an educational campaign promoting the use of slow IV push administration for clinically appropriate antibiotics including tazocin, ceftriaxone and teicoplanin. The intervention included posters, staff emails and verbal reminders during handovers, supported by guidance from the pharmacy and education teams.
Outcomes
Following the intervention, slow IV push administration increased from 40% to 82% of eligible antibiotic doses, achieving annual savings of £2,954 and 450 kgCO₂e, equivalent to driving 1,325 miles in an average car. Patient safety and care quality were maintained while treatment became faster and more efficient, supporting timely sepsis management. Staff confidence improved, with 69% choosing the sustainable option and 48% reporting increased confidence in using slow IV push. The project demonstrates how targeted education and collaboration can improve workflow, reduce waste and deliver sustainable, high-quality patient care.

“The Green Team competition proved to be a transformative experience, providing valuable resources and insights that can inform and enhance future sustainability initiatives. It underscored the synergistic relationship between economic and environmental progress, demonstrating how integrated approaches can positively impact both staff well-being and patient outcomes. I look forward to witnessing the growth and changes that stem from this.“
Nikita Baker, RN, BN, MSc Healthcare Quality, Risk and Safety, FMC Quality Improvement Consultant