
Climate change adaptation: a guide for health and care professionals
The climate and ecological crisis is degrading our planet’s life-support system and threatens our ability to thrive and survive. A bold, united response is required for both climate change mitigation and adaptation; we must reduce our contribution to the climate crisis whilst also creating resilience to respond to its impacts.
Climate change has been identified as the most important health threat of the century, but it is also the “greatest opportunity to redefine the social and environmental determinants of health”. This means that addressing both the drivers and impacts of the climate crisis is an opportunity to improve population health and places a professional imperative on those working in health and care to place climate action at the core of our practice.
What is climate change adaptation?
Adaptation refers to actions which minimise the “potential impacts of climate change, and to reduce, with the least cost, the adverse effects on health”. This means reducing the vulnerabilities of human and natural systems to the actual or expected impacts of climate change by creating system resilience. Adaptation measures are particularly crucial for social and health equity, given the worst impacts of climate change are expected to disproportionately affect those with the least ability to respond. Health and care professionals must be involved in recognising, preparing for and managing the health risks posed by climate change as a way to protect population health.
The Climate Change Act of 2008 places a requirement on the UK government to undertake 5-yearly climate change risk assessments and to put forward a UK National Adaptation Plan. The health and care sector has a responsibility to identify and act on its climate adaptation needs and has highlighted heatwaves, flooding and cold weather as particular hazards to both service disruption and increased morbidity and mortality.
Three ways to adapt to climate change in the health sector
1. Identify and monitor risks
Establishing health information systems which identify, assess and set up ongoing monitoring of specific climate risks is essential for climate adaptation. These risks can relate to both specific climate impacts, such as the likelihood of coastal or river flooding as well as the ability of the local population to adapt to adverse weather events, for which prevalence of co-morbidities, deprivation data or other vulnerability indicators should be gathered. This can be achieved through climate vulnerability and adaptation assessments, but also through closing the gaps in climate and health research. The Greener NHS currently has plans to make information on local climate risks available through a dashboard aiming to support adaptation strategies. This will allow NHS staff as well as public service decision-makers to build the capacity to respond to the specific risks and likely climate impacts on their local population.
- Heatwave and Cold Weather Plans to be replaced by a Single Adverse Weather and Health Plan
- Work with local authorities to identify and log potential risks to service continuity and population health-clinicians can do this with their individual population cohort eg. Kidney disease - at risk of heat stress - what risk management is put in place - patient education for hot days
- Undertake site reviews where hospitals are at risk of flooding, or sewage flooding is an issue, or coastal environments/other areas prone to drought or wildfire
- What site improvements need to be undertaken now for resilience to heat stress?
2. Build resilience to service disruption
One of the most important climate risks to the health sector is the disruption of coordinated health services, which affects access, coverage, continuity of care and care quality. This can be the result of major infrastructure damage (eg. road networks, energy and IT systems), as well more localised extreme-weather impacts such as flooding to individual healthcare facilities or staff shortages related to travel disruptions. The supply of medical equipment and medications in a complex and often international supply chain is also threatened by the increasing frequency of global extreme weather. There are already a number of specific plans, such as the Cold Weather or Heatwave Plan which should be put in place by health sector leads with risks and plans communicated to frontline staff.
3. Prepare the health workforce to respond to climate health impacts
Education for healthcare workers of the specific risks to health of climate impacts such as flooding, heatwaves, wildfires or changing patterns of vector-borne disease are required to reduce the expected excess morbidity and mortality related to such events. For example, increases in mosquito and tick-borne disease in the UK means UK health workers must be trained to increase their familiarity of the signs, symptoms and treatment of these diseases. Equally, healthcare workers will be required to prepare and respond to the mental health impacts of climate change which are expected to be significant, with populations affected by flooding demonstrating increased levels of depression, anxiety and PTSD and eco-distress particularly prevalent among younger age groups.
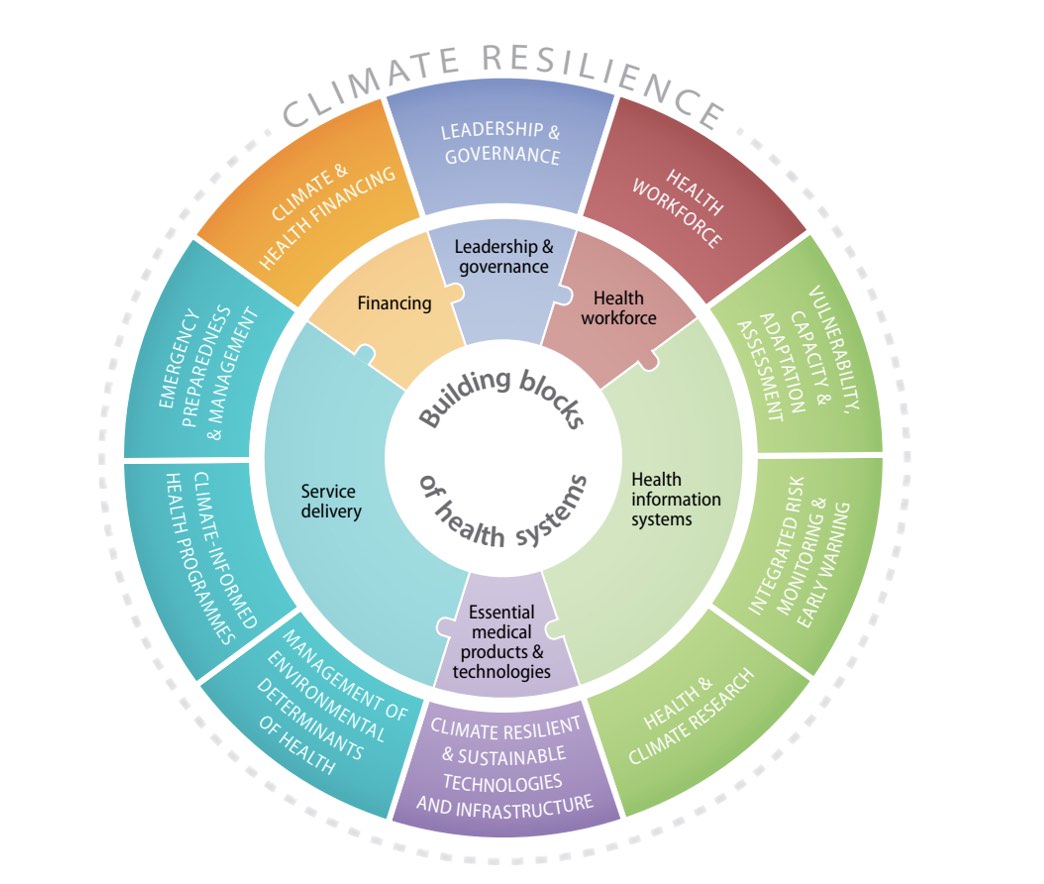
Figure 3: This figure shows the adaptation strategies related to the health system building blocks which are required for building climate resilience | Image source
Adaptation Strategies for front-line health and care professionals
- Identify patients and patient groups within your care who are at risk of climate impacts eg, air pollution spikes, cold weather, hot weather. Whilst everyone is at risk of climate change- particularly extreme weather events-the frail and elderly, young children, pregnant women and those with pre-existing co-morbidities are most vulnerable. Health workers need to understand the specific risks for the patients they look after.
- Provide information to patients and staff about protecting their health against climate change impacts
- Avoid strenuous outdoor exercises on poor air quality days for those with chronic respiratory conditions or other vulnerabilities
- Keeping cool in hot weather
- Keeping well in cold weather, as keeping your home warm
- Work with colleagues and across departments to learn more about building capacity within care pathways to deal with disruption to services
- Be alert to the mental health impacts of climate change, including eco-distress depression/anxiety/PTSD related to flooding, etc
Adaptation Strategies for managers and strategic leads
- Implement recommendations from existing climate change response plans
- Co-ordinate local action across sectors for resilience in the health and care sector (such as hospital preparedness for extreme weather events such as flooding or storms), drawing on evidence of climate risks
- Work with local authorities to find out which social groups are vulnerable, and identify suitable interventions
- Review the national or London area climate risk mapping tool
- Support Health and Wellbeing boards to build adaptation actions into local needs assessments
- Understand local climate risks such as flooding and coastal erosion
Education about the climate crisis for health professionals
- This 2-minute video from the Lancet Countdown on Health and Climate change report highlights how climate change is a critical public health issue
- Free e-learning modules on Environmentally Sustainable Healthcare e-LFH platform
- WHO online module on Human Health and Climate Change
- UK Government report on the health effects of climate change in the UK
- The Health Argument for Climate Action-WHO Special report
- A webinar series with lectures on climate change, COVID-19 and sustainability
- IPCC report on climate change
- This report by Medact outlines the public health case for Green New Deal and is an argument for social and economic structure changes to tackle climate change and social injustice
- The Met Office offers free climate projections e-learning course and climate change risk assessment training
‘Win-win’ strategies for improving public health and acting on the climate crisis
Transportation
- This guide can be used to communicate the health impacts of air pollution
- Social prescribing for active travel toolkit
- Use these resources to promote physical activity among patients: Get Active, Physical Activity Frameworks, Physical Activity Guidelines
Housing
- NICE guideline on the health impacts of cold homes
- Marmot Review on the health impacts of fuel poverty
- This resource can be provided to patients to help them make their homes more energy efficient
Food
- This brief for healthcare professionals outlines specific interventions for promoting diets that are healthy for patients and good for the planet
- This is a toolkit of information, graphics, tools and links to help you learn more about environmentally sustainable diets and how to discuss this with your patients
- Best practice examples of sustainable food for healthcare
- Circular economy for food in healthcare model
- Sustainable Food and the NHS recommendations from the King’s Fund
Green space
- Nature-Based interventions, including Green Social prescribing, walking for health and green space for health
- Nature-Based Interventions for Mental Healthcare
- Green health routes
Social inequalities
- London’s climate risk mapping training on how to consider at-risk populations
- Reducing health inequalities resources
Reducing the impact of health and care
- WHO Strategy on environmentally sustainable healthcare
- The Clean Air Hospitals Framework can be used to reduce the air pollution at hospital sites for the benefit of patients, staff and the wider community
- A list of actions local authorities can take to reduce emissions
- The UK Climate Impacts Programme toolkit to help local authorities prepare for the impacts of climate events on organisations and services
- Reduce the carbon footprint of inhaler prescribing using this guide developed by Greener Practice
- Easy wins for improving energy efficiency through behaviour change in your place of work
- Simple steps doctors can take to reduce pharmaceutical pollution
- Green Impact for Health Toolkit: resources and ideas for improving the sustainability of primary care services
Adaptation
- The WHO Operational Framework for building climate-resilient health systems
- NHS England Third Health and Care Adaptation Report
- A policy for NHS Scotland for climate emergency action
- A Welsh Government 5-year policy to adapt to climate impacts
- A toolkit to support Health and Wellbeing boards to build climate change action into Needs Assessments and Wellbeing Strategies
- This online tool helps public service providers to identify communities vulnerable to climate impacts and helps to guide decision-making on what actions to take
- This Local Climate Adaptation Tool generates recommendations of appropriate adaptation approaches, based on the best available evidence that will support the health and wellbeing of local people
Good practice examples
- Case studies from the Royal Devon and Exeter NHS Foundation Trust Green Ward competition: these projects embedded sustainability into quality improvement to reduce waste, inappropriate prescribing and unnecessary cannulation across departments
- Sussex Community NHS Trust chose to support and promote active travel by investing in e-bikes and electric and hybrid pool cares. See it in action here
- The ‘Gloves Off’ campaign at Great Ormond Street Hospital shows how simple changes to the way non-sterile gloves are used can significantly reduce the environmental impact of care while improving patient outcomes and experience
- The NHS Sheffield Clinical Commissioning Group shows how GP practices can use allotment gardening to provide healthy food to their communities and improve wellbeing
- Dorset Integrated Care System (ICS) integrated climate action into their 5-year plan (2019-2024), improving the sustainability of their service and providing care in a way that both protects and recognises the health benefits of nature and the environment. They have made particular progress on leading a whole systems approach to increasing physical activity, a key component of increasing active travel and reducing transport-related climate impacts and ill health.
- The Greater Manchester Health and Social Care Partnership manifesto uses the health voice to support a transport system which makes active travel the easy and accessible choice
- The Yorkshire and Humber Climate Commission brings public, private and third sector organisations together to prevent and prepare for the worst impacts of climate change whilst improving population wellbeing
Author
Victoria Stanford
Victoria Stanford is the 2021-2022 QI Education Fellow at CSH, working with universities and postgraduate education programmes to support the integration of sustainable healthcare into Quality Improvement teaching

