In May 2025, Norfolk and Norwich University Hospitals NHS Foundation Trust (NNUH) commenced a Green Team Competition in partnership with the Centre for Sustainable Healthcare.
The Green Team Competition is a clinical leadership and engagement programme for NHS organisations wishing to improve the sustainability of their services. Through the programme, six clinical teams at NNUH were supported by CSH to identify, plan, implement and measure quality improvement projects using the Sustainability in Quality Improvement (SusQI) methodology.
At the Showcase event on 16 September 2025, the teams presented their projects, including the financial, environmental and social outcomes achieved, as well as opportunities for next steps.
Project support and implementation
CSH has worked directly with six clinical teams across NNUH to support them in delivering greener, higher-value care through the application of the Sustainability in Quality Improvement (SusQI) methodology. By combining clinical insight with practical mentoring, teams were guided to explore how their services could improve health outcomes while reducing environmental and social costs. Using the sustainable value equation as a foundation, four teams progressed to active project delivery, developing, implementing, and evaluating initiatives that bring meaningful, measurable change in line with wider sustainability goals.


“’I’ve been following the Green Team competitions at CSH for many years and I was so excited when our charity generously funded our own competition. From the start it has been so inspiring to follow the teams and learn from the expertise of those at CSH. Following our showcase event we are thinking of how to roll these ideas out across the trust to expand on the excellent projects even further.”
Dr Amy Greengrass BM FRCA, Consultant Paediatric Anaesthetist, Clinical Lead for Sustainability
Showcase Event
At the 16 September Showcase Event, six clinical teams from Norfolk and Norwich University Hospitals presented their sustainability projects, outlining their achieved and anticipated savings, lessons learned, and opportunities to scale and spread.
The event was attended by colleagues from across the Trust and a judging panel including:
- Dr Mike Irvine, Clinical Director (Planned Care), NNUH
- Eva Zaprel, Patient Panel representative, NNUH
- Patient Panel representative, NNUH
- Dr Hayley Pinto, Education and Training Lead, The Centre for Sustainable Healthcare
Projects showcased the potential for improving clinical care while reducing environmental, financial and efficiency costs. Many also demonstrated benefits to staff and patient wellbeing, safety and experience.
The impact
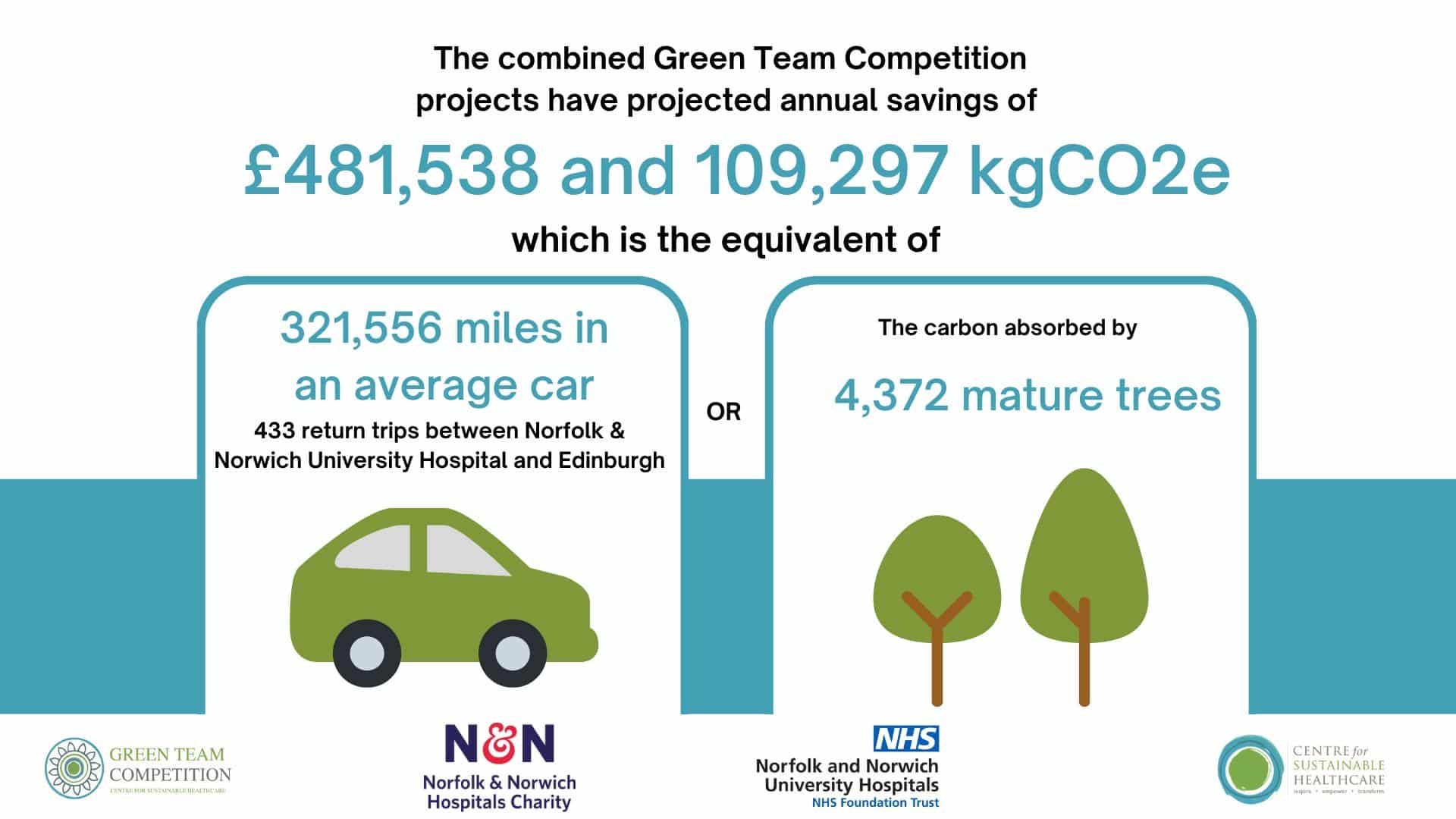
The Green Team Competition has brought meaningful, measurable value to NNUH. Collectively, the projects delivered through the competition are forecast to achieve £481,538 in annual cost savings and cut carbon emissions by approximately 109,297 kgCO₂e each year.
That’s the environmental equivalent of:
- Driving more than 321,556 miles in an average car
- Completing roughly 433 return journeys between Norfolk & Norwich University Hospital and Edinburgh
- The annual carbon absorption of around 4,372 mature trees
More than just numbers, the programme has helped ignite a culture of sustainability across clinical teams, encouraging greener, smarter, and more person-focused ways of delivering care.

“This was such an uplifting event, all the teams did so well and it was really inspiring. Just to say CSH were absolutely brilliant throughout and were really supportive so thank you to you too!”
Coco (Hiroko Spooner), Clinical Quality Improvement Lead for Medicine
These early successes show the potential of grassroots, well-mentored initiatives to support the NHS’s net zero ambitions while improving patient outcomes and operational efficiency.
Winners
Congratulations to the winning team, the Hand Surgery Team
Their project introduced a series of sustainability-focused improvements to scrubbing and post-operative procedures within the Norwich Hand Unit. Inspired by a desire to make surgical practice more environmentally responsible, the team achieved meaningful change in a short period of time.

“Ideally, this will help create a clear-cut template for more sustainable surgery practices and encourage other teams to adopt similar approaches. Reducing health inequalities by lowering transport costs for those more socially and financially deprived is also very important to us. We hope that interventions such as this will help lower the barriers people face in accessing safe and effective healthcare.”
Samuel Norton, NNUH Hand Surgery Team
With patient safety and quality of care at the forefront, their work has reduced waste, strengthened team engagement, and embedded sustainable practices into everyday clinical routines—delivering measurable environmental, financial and cultural benefits.
Highly Commended
Congratulations to the Emergency Department Nursing Team for their project, which promoted the use of slow IV push administration of antibiotics in place of saline bag infusions. This approach enhances clinical efficiency and patient comfort while significantly reducing environmental impact by cutting down on single-use plastics.
The project stands out for its strong alignment with NHS sustainability goals and its evidence-based approach to improving care delivery. It provides a compelling case for scaling similar practices across other departments and services, demonstrating how small changes can lead to meaningful environmental and clinical gains.
The Centre for Sustainable Healthcare would like to thank and congratulate all teams that took part in the competition. The outcomes of the competition stand as a testament to the dedication and innovation of each team in advancing the sustainability of healthcare at NNUH.

“The intervention has been more about education and trying to encourage nurses to choose slow IV push […] We believe the project could save staff time, as well as set up the groundwork to utilise a similar process with other drugs that we commonly use.”
TK (Theophilus Kusi) Nuamah, Registered Nurse, NNUH Emergency Department (ED) Nursing Team
Samuel Norton: “Ideally, this would help us to create a clear-cut template for more sustainable surgery practices within our Trust and encourage other teams to adopt similar practices […] Reducing health inequalities by reducing the cost of transport for those more socially and financially deprived is something that is also very important to us. We hope that interventions such as this will help lower the barriers people face in accessing safe and effective healthcare.”
Green Team Competition projects
Read the full Impact Report here or view the project summaries below.
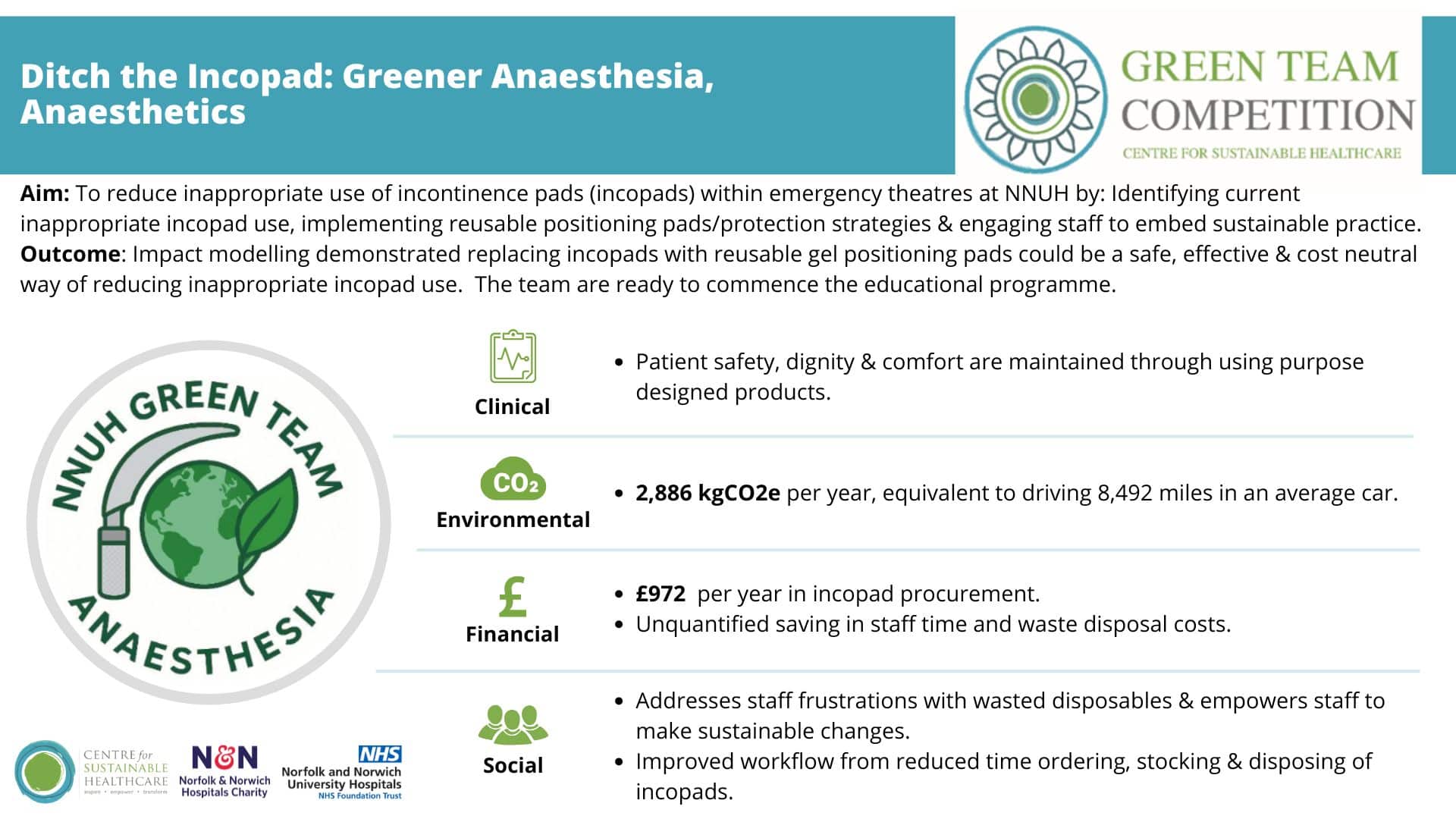
1. Ditch the Incopad: Greener Anaesthesia, Anaesthetics Team
Team members:
- Dr Ricky Lewis, ST7 Anaesthetics
- Dr Sameen Kausar, ST4 Anaesthetics
- Dr Amy Greengrass, Consultant Anaesthetist
Setting / patient group:
Patients undergoing emergency theatre procedures.
Summary
The team identified the widespread use of single-use incontinence pads (“incopads”) in theatres, often for non-clinical purposes such as patient positioning and trolley protection. To address this, they introduced reusable gel pads as a sustainable alternative. The project involved assessing baseline use, engaging staff through surveys and education sessions, and embedding reusable options into everyday practice. This intervention reduced waste, improved workflow efficiency, and maintained patient comfort and safety.
Outcomes
By replacing disposable incopads with reusable gel pads, the team anticipates annual savings of £972 and 2,886 kgCO₂e, equivalent to driving 8,492 miles in an average car. Staff report increased motivation to adopt sustainable practices, reduced frustration with waste, and smoother workflows from less time spent ordering, stocking and disposing of incopads. Patient safety and dignity are maintained, demonstrating a scalable, cost-neutral model for all theatres at NNUH.
2. Reducing patient travel by providing “same day” ultrasound and nuclear medicine appointments, Radiology Department Team
Setting / patient group: Radiology services for paediatric patients requiring ultrasound and nuclear medicine scans.
Summary
Children undergoing kidney assessments at NNUH often need both ultrasound (US) and nuclear medicine (NM) scans. Historically, these have been booked on separate days by different teams, resulting in extra travel, higher costs for families, and increased carbon emissions. The team worked to align scheduling, engaging referrers to request both tests simultaneously, introducing a “same day” booking template, and reserving ultrasound slots for eligible patients. This initiative improved patient experience, reduced travel, and demonstrated the feasibility of integrated scheduling for imaging services.
Outcomes
Eight out of ten participating patients successfully received same-day scans, avoiding additional travel and saving an estimated 88.18 kgCO₂e, equivalent to driving 232 miles. Extrapolated across eligible patients, annual savings could reach 594.6 kgCO₂e and 2,013 miles avoided. Parents valued the convenience, with an estimated 88 school or workdays saved. The approach was cost-neutral, with potential efficiency gains from reduced DNA rates and streamlined bookings. Staff engagement increased, inspiring further sustainability-focused improvements in radiology scheduling.
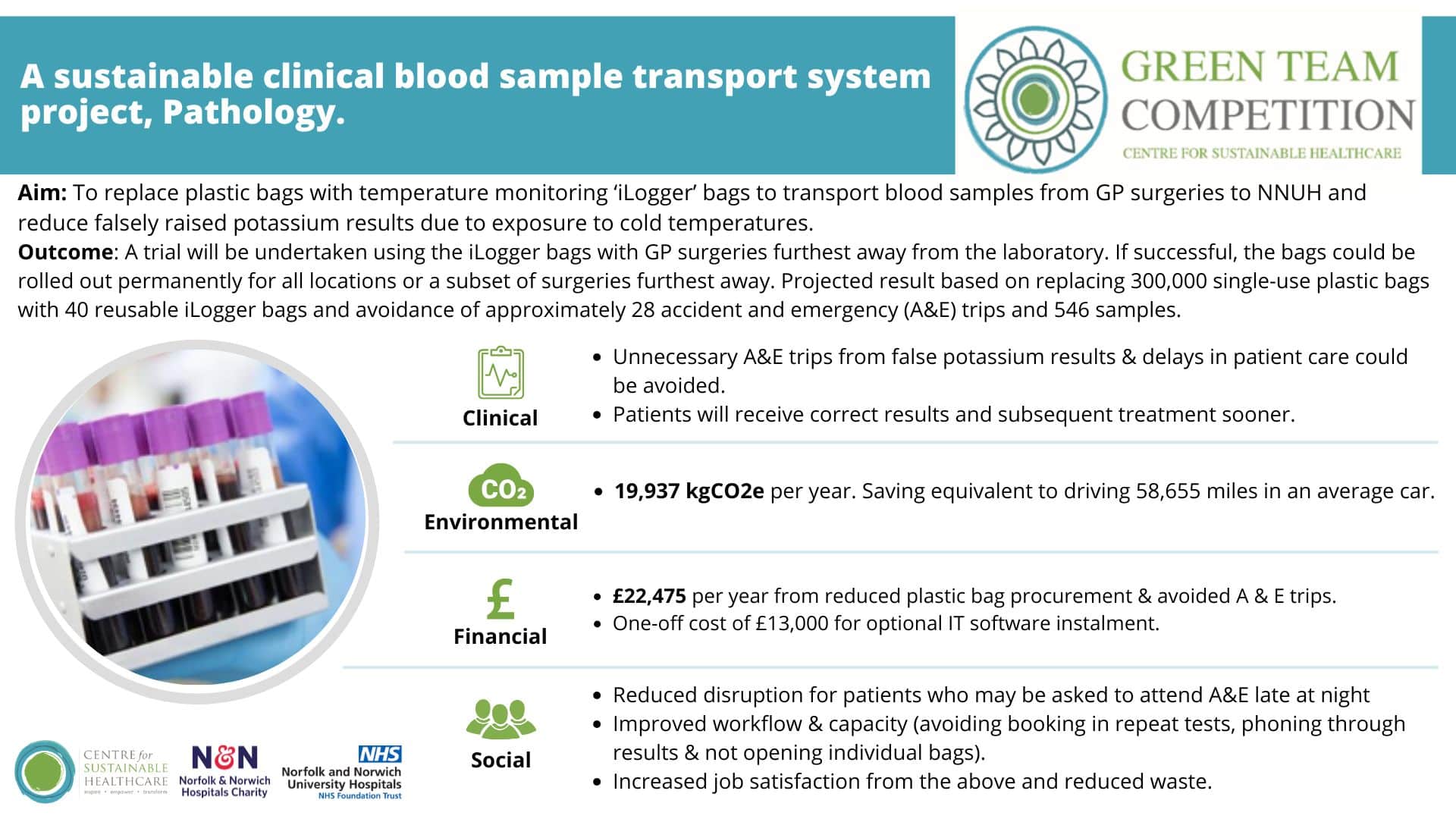
3. A sustainable clinical blood sample transport system, Pathology Team
Team members:
- Laura Cook, Clinical Scientist
- Emma Miler, Clinical Scientist
- Bitzy Cave, Biomedical Scientist
- Emily Leach, Clinical Scientist
- George Bailey, Pre-Analytics Manager
Setting / patient group: GP surgeries from North Norfolk and Norwich requiring potassium blood samples to be delivered to the Eastern Pathology Alliance (EPA).
Summary
The team identified high numbers of falsely raised potassium results from GP surgeries in North Norfolk during winter months, caused by cold exposure during sample transport. This led to unnecessary hospital visits, repeat tests and increased waste due to single-use plastic packaging. To address this, the team trialled reusable insulated iLogger bagsequipped with temperature monitoring technology. These bags maintain optimal temperatures during transit and provide data integration with the laboratory IT system, ensuring accuracy and improving efficiency.
Outcomes
Replacing 300,000 single-use plastic bags with 40 reusable iLogger bags is projected to save 19,937 kgCO₂e annually, equivalent to driving 58,655 miles in an average car. Financial savings of £22,475 per year are anticipated through reduced consumable costs and fewer unnecessary A&E visits. Clinically, the project will prevent false potassium readings and improve equity of care for patients in rural areas. Staff benefit from reduced waste handling, improved workflow, and greater job satisfaction. The approach offers a scalable, low-cost solution with significant environmental and patient care benefits.
4. Rehabilitation Assistants in supporting the recovery of critical care step-down patients, Recognise and Response Team (RRT).
Team members:
- Annie Sturrock, RRT Lead for Quality Assurance and Education
- Alanna Forrester, RRT Clinical Lead
- Laura Grimsey, CCC Clinical Lead Physiotherapist
Setting / patient group: Patients stepping down to the ward after spending more than 72 hours in critical care.
Summary
Patients leaving critical care often face physical, psychological and cognitive challenges, yet therapy input typically decreases after transfer to the ward. To bridge this gap, the team introduced structured rehabilitation support delivered by rehabilitation assistants for patients who had spent over 72 hours in critical care. The assistants rotated between critical care and ward settings to maintain continuity of care and ensure familiarity with each patient’s journey, improving both recovery and patient experience.
Outcomes
The project reduced the average hospital stay after critical care discharge by three days, saving approximately 1,734 bed days and £422,435 annually. Environmental savings total 64,598 kgCO₂e, equivalent to driving 190,050 miles in an average car. Patients reported improved wellbeing, reassurance and motivation through seeing familiar staff, while rehabilitation assistants felt valued and supported in their extended role. The initiative demonstrates how continued therapy after critical care can enhance recovery, reduce resource use, and improve both patient and staff experience.
5. Encouraging slow IV push of antibiotics (tazocin, teicoplanin, ceftriazone) instead of saline bag administration, Emergency Department (ED) Nursing Team
Team members:
- TK (Theophilus Kusi) Nuamah, Registered Nurse
- Isaiah Onumah, Registered Nurse
- Paul Welander, ED Matron
Setting / patient group: Patients requiring IV antibiotics in the Emergency Department.
Summary
The team identified a long-standing reliance on 100 ml saline bag infusions for administering IV antibiotics in the Emergency Department, contributing to excess plastic waste, higher costs and potential treatment delays. To address this, they launched an educational campaign promoting the use of slow IV push administration for clinically appropriate antibiotics including tazocin, ceftriaxone and teicoplanin. The intervention included posters, staff emails and verbal reminders during handovers, supported by guidance from the pharmacy and education teams.
Outcomes
Following the intervention, slow IV push administration increased from 40% to 82% of eligible antibiotic doses, achieving annual savings of £2,954 and 450 kgCO₂e, equivalent to driving 1,325 miles in an average car. Patient safety and care quality were maintained while treatment became faster and more efficient, supporting timely sepsis management. Staff confidence improved, with 69% choosing the sustainable option and 48% reporting increased confidence in using slow IV push. The project demonstrates how targeted education and collaboration can improve workflow, reduce waste and deliver sustainable, high-quality patient care.
6. Hand Unit Greener Surgery, Hand Surgery Team
Team members:
- Mr Samuel Norton
- Mr Ken Wong
- Miss Jasmine Crane
- Mr Thomas Barber
- Miss Rebecca Fish
- Miss Dominique Dennis
Setting / patient group: Patients undergoing hand surgery in the NNUH Ambulatory Procedure Unit (APU).
Summary
Recognising that surgical activity contributes up to 30% of total hospital waste, the Hand Surgery Team set out to reduce the environmental impact of their procedures while maintaining high-quality patient care. The project focused on replacing single-use items with reusable alternatives, streamlining surgical packs, and eliminating unnecessary consumables. Key actions included switching from visored to standard masks, introducing reusable gowns and hats, transitioning to hand sanitiser for scrubbing, and removing routine post-operative prescriptions for simple analgesia and bottled water provision.
Outcomes
The project achieved an estimated annual saving of £32,702 and 20,831 kgCO₂e, equivalent to driving 61,286 miles in an average car. No adverse impact on patient care was reported, and staff morale improved through increased environmental awareness and efficiency gains—such as reduced scrubbing time and simplified workflows. The initiative demonstrates that substantial environmental and financial benefits can be achieved without compromising safety or standards, highlighting the impact of strong team engagement and education in sustainable surgical practice.

“It’s great to see what teamwork can produce. Together we’ve shown that we can be a leaner, greener and more sustainable regional hand service whilst maintaining the same high level of care.”
Rebecca Fish, NNUH Hand Surgery Team