In May 2025, Wrightington, Wigan and Leigh (WWL) Teaching Hospitals NHS Foundation Trust commenced a Green Team Competition in partnership with the Centre for Sustainable Healthcare.
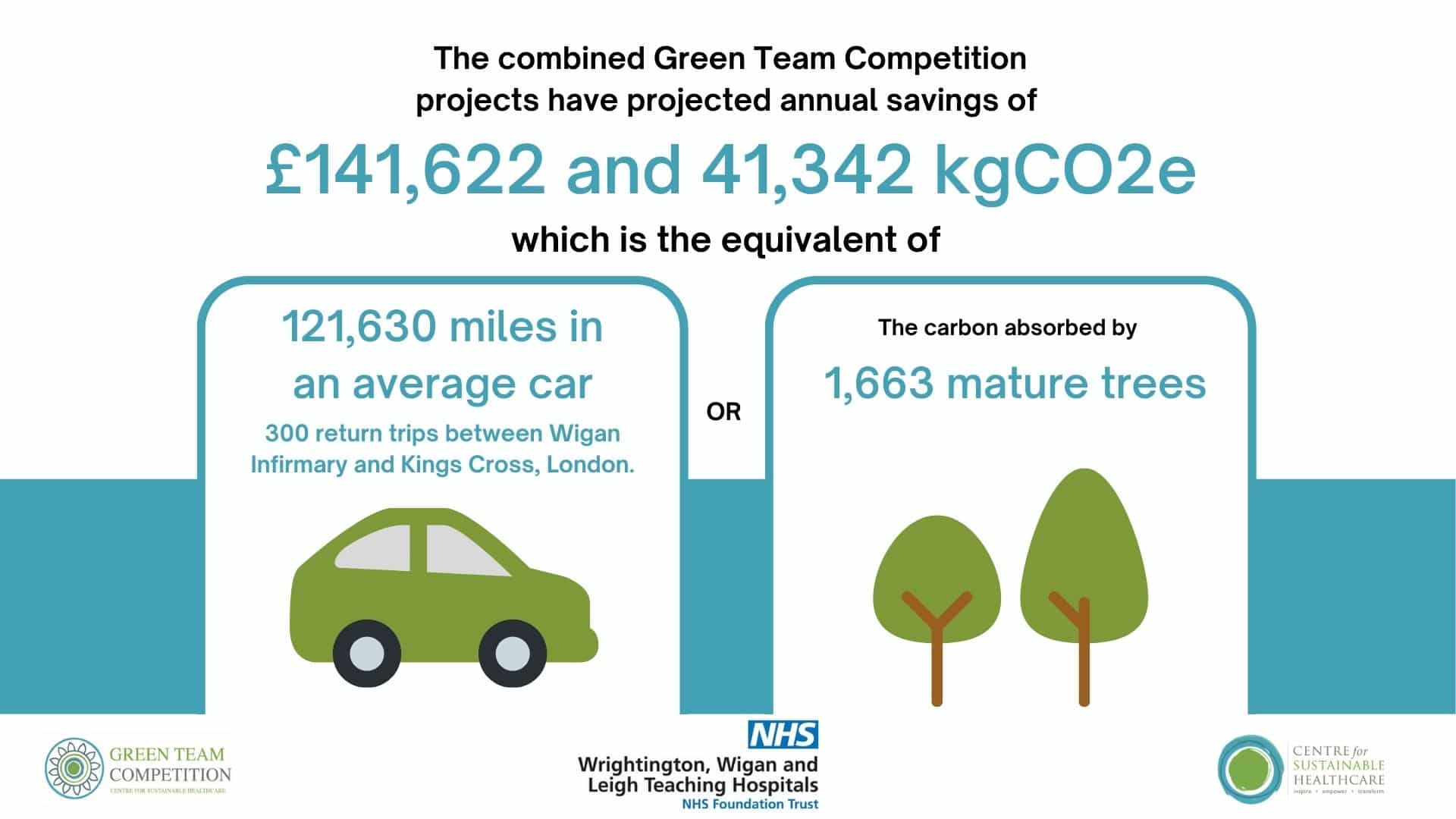
Through this latest Green Team Competition, projects across WWL are projected to deliver annual savings of £141,622 and reduce carbon emissions by 41,342 kgCO2e, the equivalent of driving 121,630 miles in an average car.
Building on staff enthusiasm for sustainability, participants received expert guidance through the Centre for Sustainable Healthcare’s award-winning Sustainability in Quality Improvement (SusQI) framework. This structured approach enabled teams to design, implement and assess initiatives that deliver measurable environmental, financial and patient care benefits, embedding sustainable thinking into everyday healthcare improvement.
Project support and implementation
CSH has worked directly with six clinical teams across WWL to support them in delivering greener, higher-value care through the application of the Sustainability in Quality Improvement (SusQI) methodology. By combining clinical insight with practical mentoring, teams were guided to explore how their services could improve health outcomes while reducing environmental and social costs. Using the sustainable value equation as a foundation, four teams progressed to active project delivery, developing, implementing, and evaluating initiatives that bring meaningful, measurable change in line with wider sustainability goals.

Showcase Event
At the September 2nd Showcase Event, the teams presented their projects, including the anticipated savings and opportunities to scale and spread, to an audience from the Trust and the judging panel including:
- Richard Mundon, Deputy Chief Executive
- Josh Balmer, Environmental and Sustainability Manager
- Harriet Attwell-Rogers, EU Horizons Project Manager, Centre for Sustainable Healthcare
Projects showcased the potential for improving clinical care while reducing environmental, financial and efficiency costs. Benefits to both staff and patient wellbeing and experience were also achieved.
The impact
The Green Team Competition has brought meaningful, measurable value to WWL. Collectively, the projects delivered through the competition are forecast to achieve £141,622 in annual cost savings and cut carbon emissions by approximately 2841,342 kgCO2e each year. That’s the environmental equivalent of:
- Driving 121,630 miles in an average car (unknown fuel).
- Completing roughly 300 return journeys between Wigan Infirmary and Kings Cross, London.
- The annual carbon absorption of 1,663 mature trees
More than just numbers, the programme has helped ignite a culture of sustainability across clinical teams, encouraging greener, smarter, and more person-focused ways of delivering care.
These early successes show the potential of grassroots, well-mentored initiatives to support the NHS’s net zero ambitions while improving patient outcomes and operational efficiency.
Winners
Congratulations to the winning team, the Community Transformation Team
Their new approach to wound care, inspired by a similar initiative in another NHS trusts, ensures that dressings are now available at the point of need, eliminating the delays associated with prescriptions. With patient care and equitable access at the heart of the project, they’ve also delivered significant savings in staff time, financial resources, and environmental impact.

“We have thoroughly enjoyed working on this Green Team project with CSH, the support and guidance was excellent. It was also fantastic to hear the presentations from the other project teams within the Trust and to listen to their ideas. It has certainly raised our awareness of sustainability and made us start to consider what else could be implemented to be greener within our division to reduce our carbon footprint whilst making improvements for our patients, staff and organisation.”
Elaine McDowell, Head of Business Development & Transformation, Community Division, WWL
At the Centre for Sustainable Healthcare, we’re excited to follow the team’s progress as they work towards scaling this impactful initiative beyond their Treatment rooms, to community nursing teams.
Highly Commended
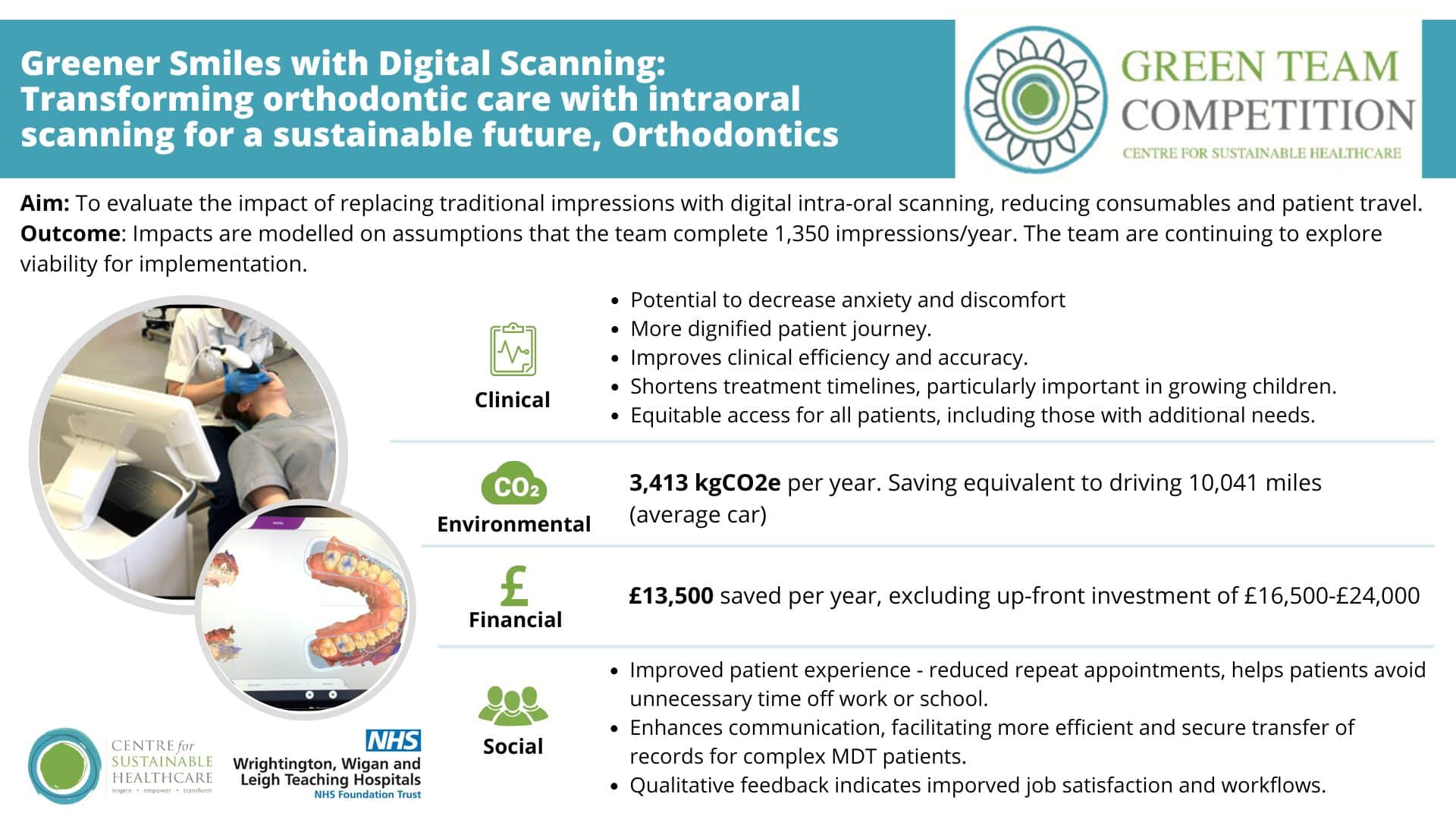
Congratulations to the Orthodontics Team for their project, which evaluated the impact of replacing traditional impressions with digital intra-oral scanning. This not only enhances patient experience and clinical efficiency but also significantly reduces environmental impact by cutting down on single-use consumables. The project stands out for its clear alignment with NHS sustainability goals and its potential to scale across orthodontic (and other) services. The project provides a compelling business case, laying the groundwork for future funding and implementation.
The Centre for Sustainable Healthcare would like to thank and congratulate all teams that took part in the competition. The outcomes of the competition stand as a testament to the dedication and hard work of each team in advancing the sustainability of our healthcare systems.
Green Team Competition projects
Read the full Impact Report here or view the project summaries below.
1. Community Wound Care Transformation, Community Transformation Team
Team members:
- Elaine McDowell, Head of Business Development & Transformation in the Community Division of WWL
- Paula Shenton, Project Manager, Community Transformation Team
- Emma Fisher, Team Leader, Treatment Room service
- Colin Carruthers, Community Stock Manager
Setting / patient group:
Patients requiring wound care who attend community treatment rooms.
Summary
The team transformed their community wound care service by removing the need for prescriptions and supplying dressings directly at the point of care. Previously, patients faced delays, missed appointments, and logistical challenges due to a complex prescription-based system. The pilot, launched in Treatment Rooms, introduced NHS Supply Chain ordering, standardised products via the Greater Manchester Wound Formulary, and recruited Stock Managers to oversee inventory and redistribution. This streamlined approach improves access, reduces waste, and aligns with sustainability goals.
Outcomes
Based on prescribing approximately 150,000 dressings per year, savings of £103,023 and 1,991 kgCO2e, equivalent to driving nearly 6,000 miles are anticipated. Patients benefit from reduced travel, fewer missed appointments, and no need to store bulky items. The equivalent 1.4 full-time roles are saved from eliminating prescription writing. Access and equity are improved, especially for vulnerable groups. The initiative highlights how collaborative system-wide change, supported by senior leadership and iterative improvement, can deliver sustainable value.

2. Transforming orthodontic care with intraoral scanning for a sustainable future, Orthodontics Team
Team members:
- Naomi Prado (Consultant Orthodontist)
- Laura Ewbank (Consultant Orthodontist)
Setting / patient group:
Orthodontic patients at Royal Albert Edward Infirmary, WWL NHS Trust, undergoing impression-taking for diagnosis and appliance fabrication
Summary
At Royal Albert Edward Infirmary, WWL NHS Trust, the orthodontic team evaluated the impact of replacing traditional dental impressions with digital intra-oral scanning to improve patient experience and reduce environmental impact. Traditional methods generate significant clinical waste and carbon emissions, often requiring multiple appointments and causing discomfort, especially for children and patients with sensory needs. Digital scanning offers a faster, more accurate, and patient-friendly alternative, aligning with NHS sustainability goals. Financial investment, integration with existing electronic health record systems, and staff training is required for the transition.
Outcomes
The switch to digital scanning is projected to save 3,413 kgCO2e annually, equivalent to driving over 10,000 miles, and reduce costs by £13,500 per year. With scanner costs recuperated in 2–3 years, the intervention also improved clinical workflows, staff morale, and patient satisfaction, with 70% preferring digital scans. Fewer appointments mean less time off school or work, and better service equity for complex cases.
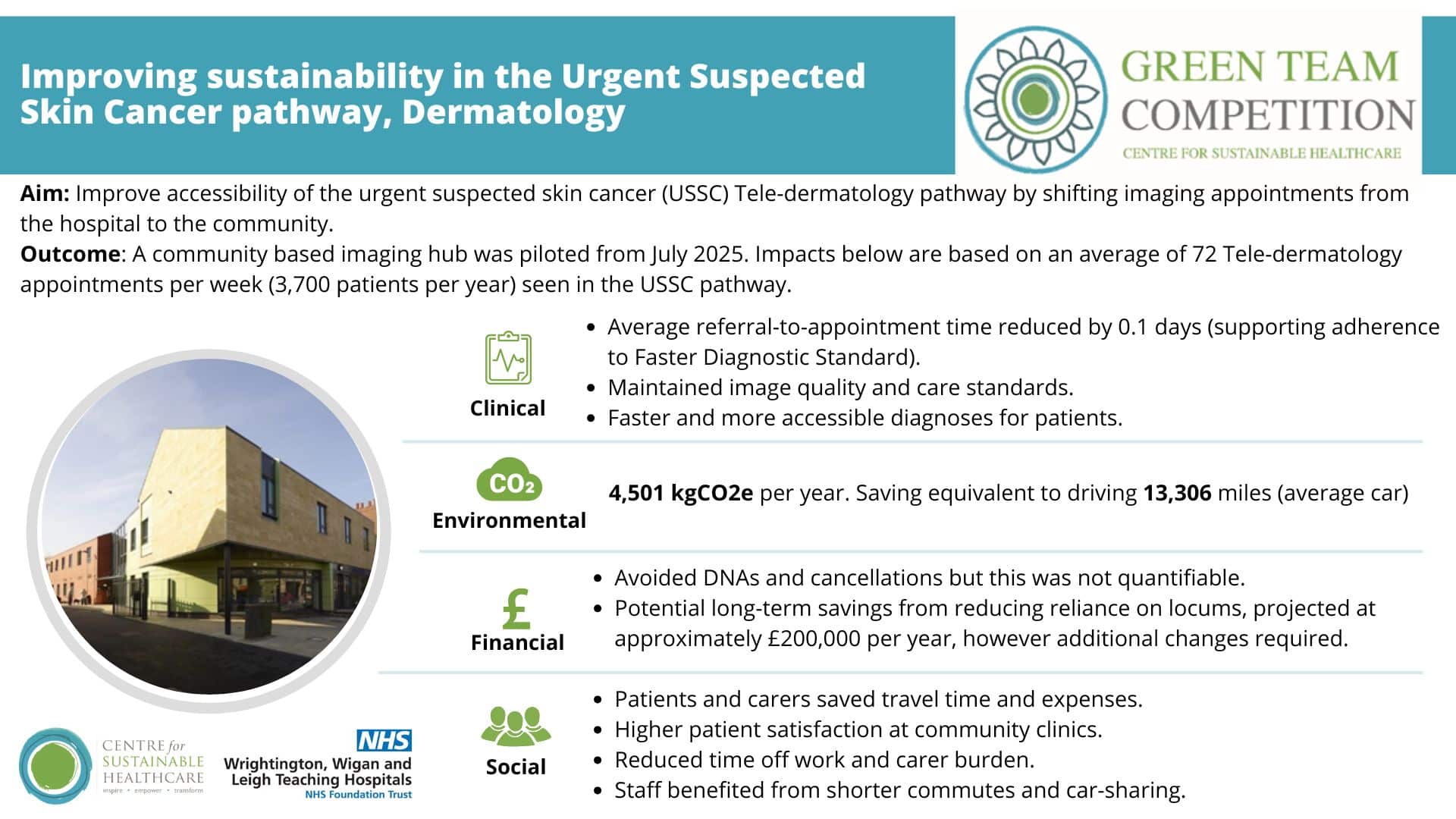
3. Improving sustainability in the Urgent Suspected Skin Cancer pathway, Dermatology Team
Team members:
- Lewis Veale (Physician Associate & Skin Cancer Pathway Specialist)
- Dr Monica Bhushan (Consultant Dermatologist & Clinical Lead for Skin Cancer)
- Andrea Jones (Head of Medical Illustration); Olivia Madden (Medical Photographer)
- Ayesha Habib (MBChB student).
Setting / patient group: Urgent Suspected Skin Cancer referrals across Wigan; community imaging hubs (Standish live; Boston House next).
Summary
To address rising demand in the urgent suspected skin cancer (USSC) pathway, the team piloted a community-based imaging hub for Tele-dermatology. Photography clinics were relocated from Leigh Infirmary to community sites. Three suitable locations were identified, improving accessibility and reducing pressure on hospital services. The pilot began in July 2025 at one site, with plans to establish the other two sites soon.
Outcomes
By supporting 3,700 patients to access their appointment closer to home, the project saves 4,501 kgCO2e per year, equivalent to driving over 14,000 miles. Patients benefit from reduced travel, reducing referral-to-appointment time, quicker diagnoses, and higher satisfaction. Staff enjoy shorter commutes and improved workflow. Though financial savings from reduced cancellations are not yet quantified, future reductions in locum reliance could save £200,000 annually. The initiative shows that decentralising diagnostics can improve access and sustainability with minimal disruption.
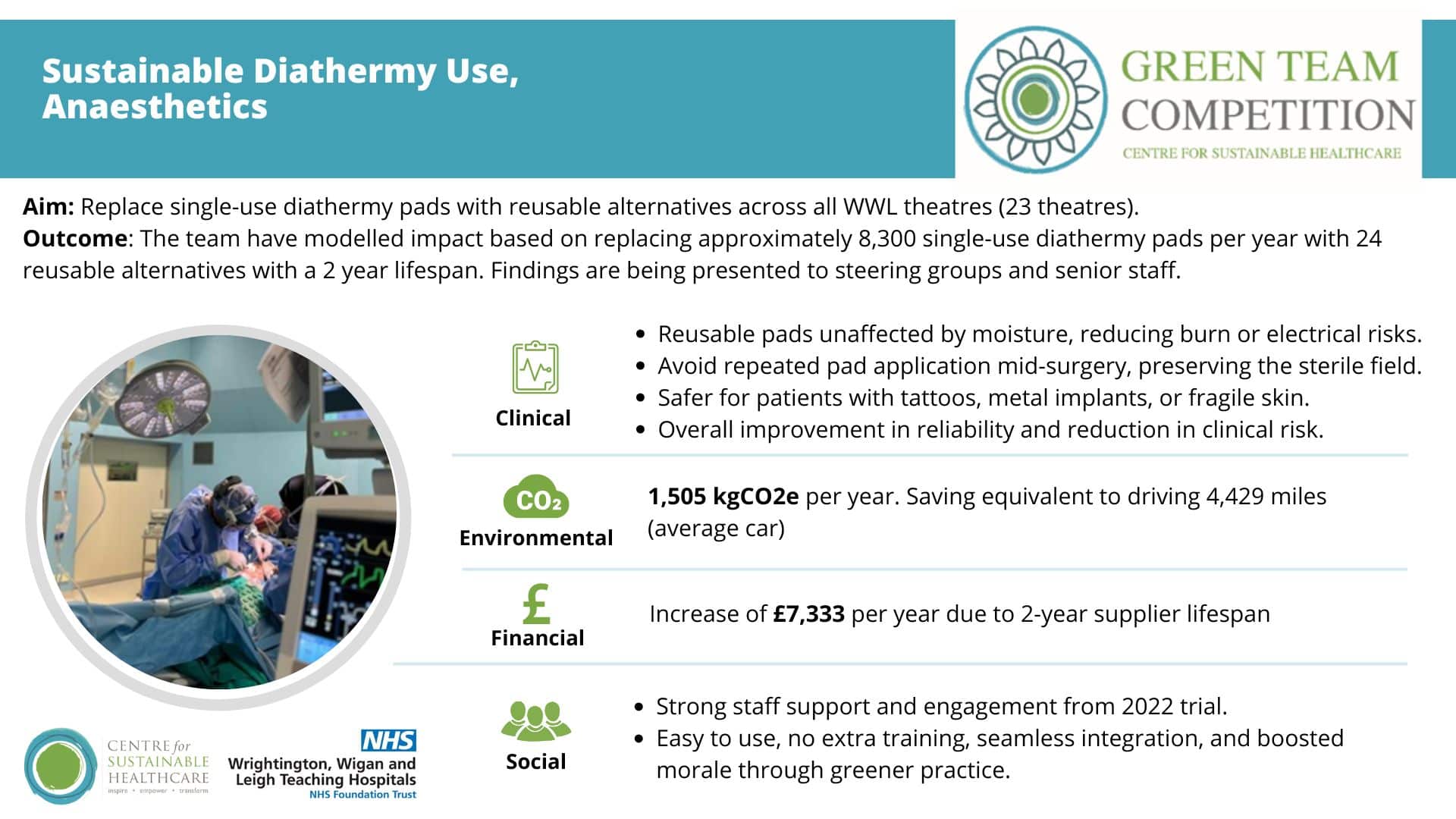
4a. Reusable diathermy return electrodes (pads), Surgery and Anaesthetics Team
Team members:
- Miss Naomi Mackenzie, Consultant Surgeon, Royal Albert Edward Infirmary, Wigan
- Miss Kerry Foley, Surgical Registrar
Setting / patient group:
Elective and day-case theatres across Wrightington, Wigan and Leigh (WWL) NHS Trust, covering 23 theatres across three hospital sites.
Summary
Theatres are planning a switch from single-use to reusable diathermy pads to reduce clinical waste and carbon emissions. A 2022 trial showed reusable pads are safe, compatible with existing equipment, and well-received by staff. The team has modelled environmental and financial impacts and is now seeking executive approval for trust-wide implementation.
Outcomes
Replacing 8,300 single-use pads annually with 24 reusable ones could save 1,505 kgCO2e, equivalent to driving over 4,400 miles. While the switch may increase costs by £7,333 per year due to fixed lifespan pricing, targeting high-use theatres could improve cost-effectiveness. Clinically, reusable pads offer greater reliability and safety (though risks were already low). Staff support greener practices with no need for extra training. The initiative highlights how sustainability and safety can align, with leadership buy-in key to success.
4b. Rationalising use of Anaesthetic Gas Scavenging (AGSS) and Ventilation Systems, Surgery and Anaesthetics Team
Team members:
- Dr Neelam Patel, Consultant Anaesthetist and Clinical Director
- Mr Marcus Summers, Head of Operational Estates
- Mr Josh Balmer, Environmental and Sustainability Manager,
Setting / patient group:
Theatres at WWL, starting with Leigh Infirmary (4 day-case theatres) and with potential for wider rollout across 23 theatres trust-wide.
Summary
AGSS is a vital part of anaesthetic practice as it removes excess volatile anaesthetic gas away from the theatre environment to protect staff within the theatre environment. Theatre ventilation and laminar flow systems regulate environmental temperature and humidity, provide a level of infection control as well as a comfortable ambient temperature to operate in. These systems were running 24/7, despite the four day-case theatres having fixed weekday hours and no overnight activity. The team assessed feasibility to implement an automatic “theatre setback mode”.
Outcomes
The intervention requires works (e.g. replacing indicator lights, rewiring), automation with manual override for overruns, and staff training to ensure safe use and adoption. Approval for the works is pending. In just 4 theatres, the initiative could save 42,191 kgCO2e, equivalent to driving over 27,700 miles. Energy costs will reduce by £19,675 in year one, increasing in subsequent years. The initiative demonstrates how operational changes can deliver significant environmental and financial benefits.
5. Transitioning to reusable cups in inpatient wards, Hotel Services and Catering Team
Team members:
- Angela Reeve – Deputy Hotel Services Manager
- Gavin Thorpe – Deputy Hotel Services Manager
Summary
Inpatient wards rely heavily on single-use cups, with each 28-bed ward at WWL using approximately 71,000 cups annually. This generates substantial waste and contributes to the Trust’s carbon footprint. While some wards had independently transitioned to reusable cups due to storage challenges, the majority continued using disposables. The team aimed to replace single use cups for drinks with reusable options for inpatients on wards who opt-in to the change.
Outcomes
Four wards signed up with initial engagement, with more expected to join. The transition supports patient comfort and ease of drinking (especially for those with dexterity issues). From just four wards, £12,757 and 2,148 kgCO2e will be saved per year, the carbon equivalent of driving 6,320 miles. Staff were surprised by the volume of single use waste generated. Initial concerns about cleaning are expected to ease as wards integrate the process into routines.
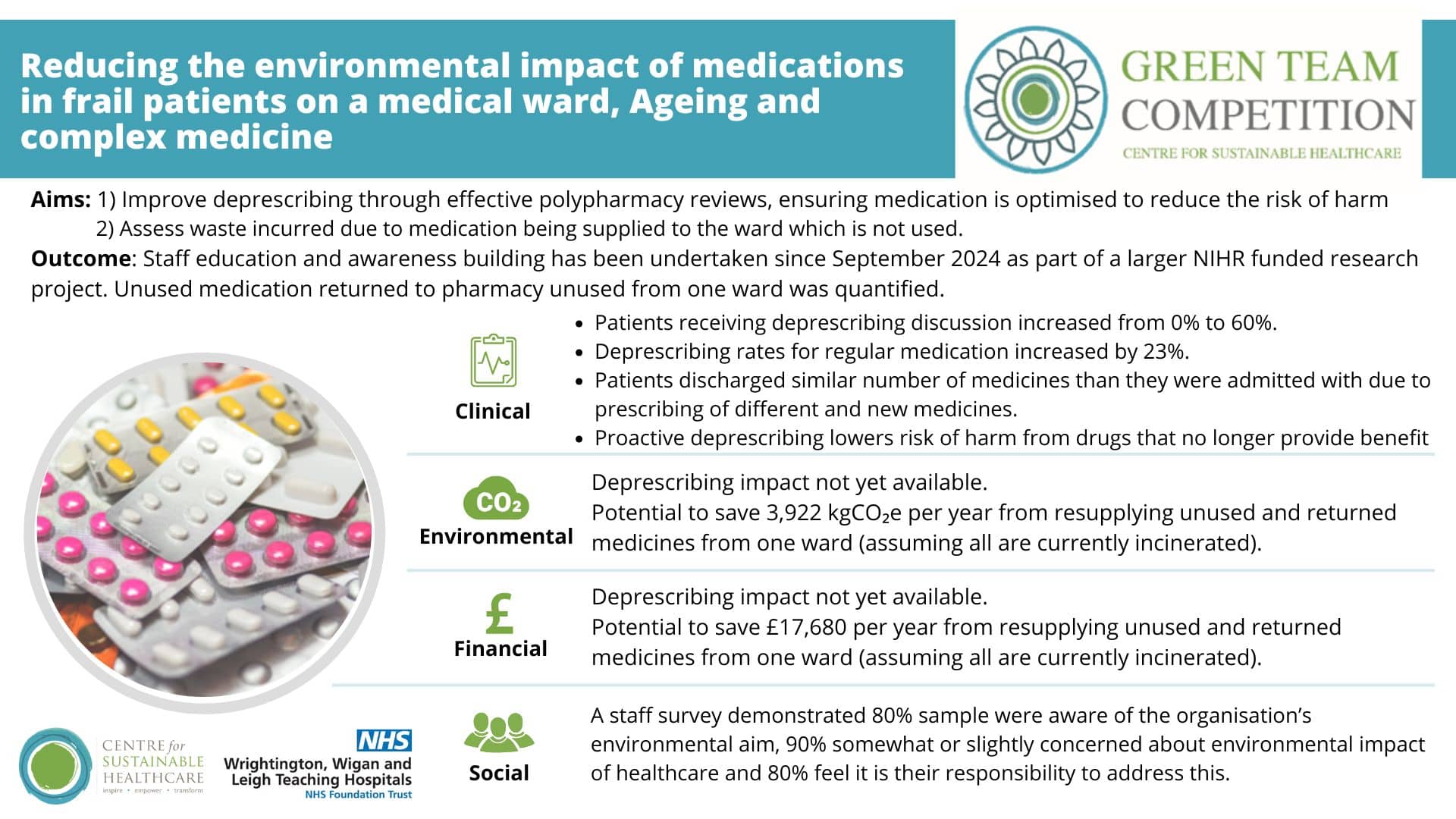
6. Deprescribing in frailty, Ageing and complex medicine team
Team members:
- Ðula Alićehajić-Bečić, Consultant Pharmacist Frailty
- Martin Farrier, Director of Digital Medicine, Chief Clinical Information Officer, Consultant Paediatrician
- Samuel Farrier, Pharmacist
- Donna Hewitt, Astley ward Manager
- Emily George and Alisha Maini, Polypharmacy analysis
Setting / patient group: Frailty Ward
Summary
Frailty wards face unique challenges in medication management, with many patients at risk from inappropriate polypharmacy. The ward joined the NIHR-funded CHARMeR study which encourages proactive deprescribing. Educational workshops were delivered to rotating doctors, consultants, and pharmacists, focusing on evidence-based deprescribing, barriers to implementation, and patient attitudes. A checklist was added to ward round notes to prompt deprescribing discussions.
The team also assessed the environmental and financial impact of unused medications that are returned to pharmacy, highlighting opportunities for more sustainable practices.
Outcomes
An increase in deprescribing rates of 23% was offset by a rise in newly prescribed medications, resulting in similar medication numbers between admission and discharge. This was due to new clinical needs and substitution within drug classes, making it difficult to determine the true financial and environmental impact of deprescribing. However, the shift toward proactive reviews marked a clinical improvement and reduces risk to patients.
There is potential to save £17,680 and 3,922 kgCO2e per year from resupplying unused and returned medicines from one ward (assuming all are currently incinerated). Further engagement with pharmacy teams is required to assess feasibility and safety or resupplying medications.