In September 2024, RUH Bath commenced a Green Team Competition in partnership with the Centre for Sustainable Healthcare. The competition has brought anticipated annual savings to the Trust of £41,000 and 50,000kg CO₂e. This is the carbon footprint equivalent of driving over 147,000 miles in an average car (or 640 return trips between Bath and London).
Supporting RUH Bath Net Zero ambition
Royal United Hospitals Bath NHS Foundation Trust is committed to reaching its net zero goals. To support this ambition, the Trust partnered with CSH to run a Green Team Competition as a way to help staff integrate sustainability into Quality Improvement Projects. Recognising that many staff members support net zero ambitions and that a great deal of good work is already taking place, the competition was designed to provide structured support, offering a clear package of knowledge, skills, and tools to facilitate positive change. The initiative aims not only to achieve financial savings but also to consider social and environmental factors while maintaining a strong focus on positive health outcomes for all.

“It has been encouraging to see the momentum that the Competition has gained for projects around the Trust, and the positive feedback for having access to this support. We are exploring how to continue this positive momentum going forwards.”
Liz Ray, Sustainability Manager, RUH Bath
Project support and implementation
Through the Green Team Competition, five teams from RUH Bath were selected to participate in our award-winning Sustainability in Quality Improvement (SusQI) programme, which transforms expert knowledge into action. Each team received mentoring from CSH facilitators to drive healthcare transformation by developing, implementing, and measuring the impact of projects through the lens of the sustainable value equation.

Showcase and awards ceremony
At the Showcase and Awards Ceremony on 10th February 2025, the teams presented their projects, including the anticipated savings and opportunities to scale and spread, to an audience from the Trust and the judging panel including:
- Sumita Hutchison, Non-Executive Director, RUH Bath
- Lisa Lewis, Head of the Coach House, Programme Lead for Improving Together, RUH Bath
- Fi Abbey, Head of Strategic Projects, RUH Bath
- Rachel Hambly, Programme Director, Improvement Programme, RUH Bath
- Rachel McLean, Sustainability in Quality Improvement Programme Lead, CSH
The impact
The Green Team Competition has delivered substantial and measurable benefits for the Trust. Across the participating projects, the initiative has generated anticipated annual savings of £41,000 and reduced carbon emissions by an estimated 50,000kg CO₂e. To put this into perspective, that’s equivalent to:
- Driving over 147,000 miles in an average petrol car
- Completing around 640 return journeys between Bath and London
- The carbon absorbed by more than 2,000 mature trees in a year
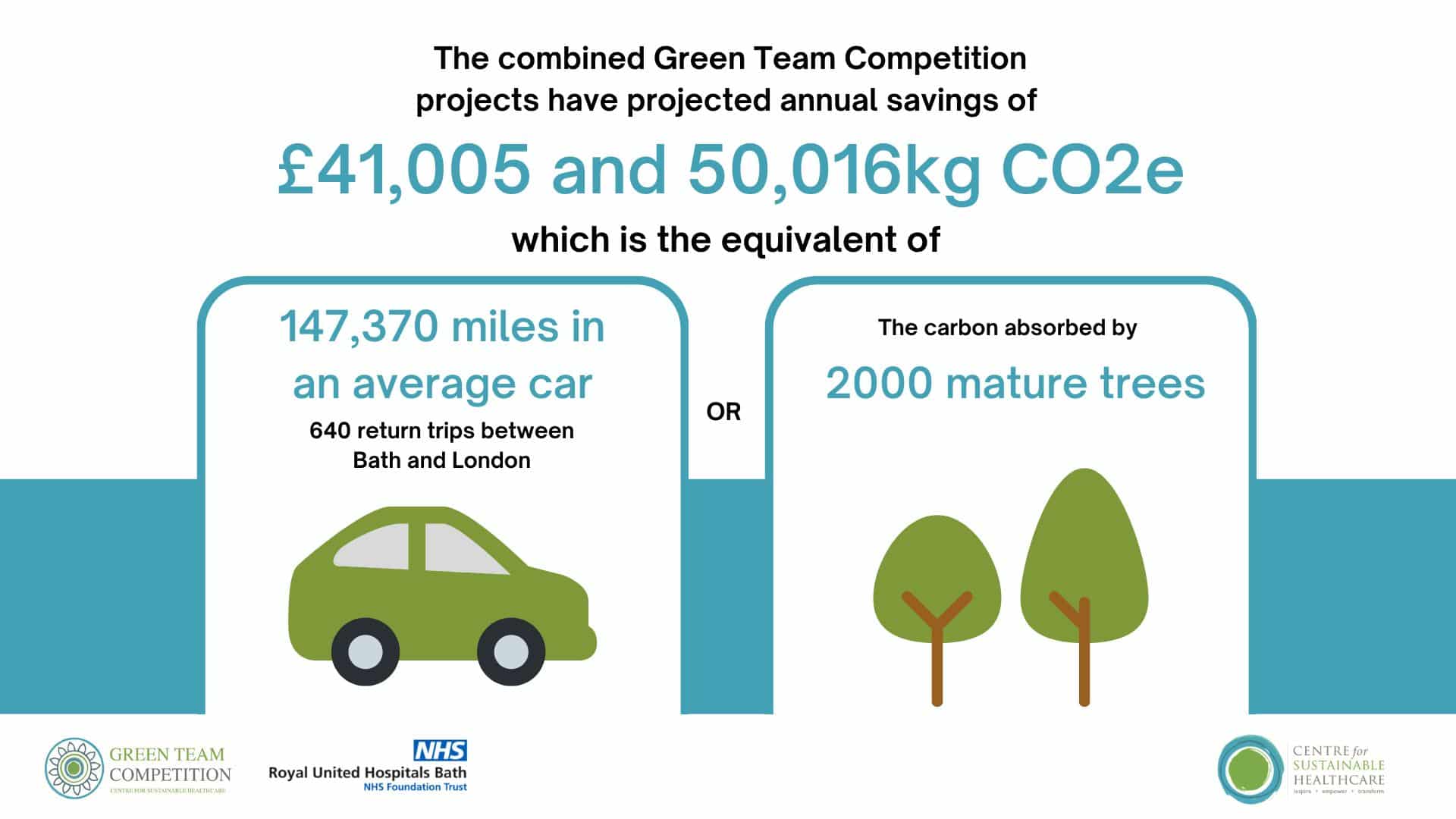
Beyond the figures, these outcomes demonstrate the potential of embedding sustainability into everyday clinical and operational practices. The projects not only achieved cost and carbon reductions but also sparked wider conversations, inspired behavioural change, and empowered teams to think critically about resource use, efficiency, and environmental responsibility within their services.
This impact reflects just a starting point: highlighting how relatively small, well-supported initiatives can scale up to make a meaningful contribution to both financial resilience and environmental goals in healthcare.
Winners
Congratulations to the winning teams, the Anaesthetics team, led by Thea Morgan, Anaesthetic Clinical Fellow and the Endoscopy Team led by Anuska Glendinning-Cranch, Clinical Endoscopist.
The Centre for Sustainable Healthcare would like to thank and congratulate all teams that took part in the competition. The competition’s outcomes serve as proof of the teams’ commitment and efforts to improve the sustainability of our healthcare systems.
Green Team Competition projects
Read the full Impact Report here or view the project summaries below.
1. Turning off the anaesthetic gas scavenging equipment in the day surgery theatre suite when not in use, Anaesthetics Team
Team members: Thea Morgan Anaesthetist RUH; Lauren Brain, Anaesthetist RUH.
Setting / patient group: Anaesthetics, day surgery.
Summary
Anaesthetics contribute significantly to the NHS’s carbon footprint, with operating theatres being particularly energy-intensive. A major factor is Anaesthetic Gas Scavenging Systems (AGSS), which often run unnecessarily when theatres are not in use. This project, in collaboration with the Estates team, focused on identifying interlinked theatres at the RUH and assessing the feasibility of turning off AGSS when not needed. Day surgery theatres, which remain unused for 118 hours per week, were chosen as the starting point since their scavenging systems can be individually isolated. While governance approval is still in progress, the initiative has been well received.
A key challenge has been assigning responsibility for switching AGSS on and off. Although the system is not yet being turned off overnight or on weekends, the project has sparked interest in broader energy-saving measures, such as reducing heating and ventilation in unused areas. Additionally, efforts are underway to reintroduce theatre checklists to ensure AGSS is managed effectively at the beginning and end of each theatre session.
Outcomes
Although no results are available yet, the project aims to track incident reporting once implemented. Environmentally, turning off anaesthetic gas scavenging in day surgery theatres when unoccupied could save around 42,191kg of CO₂ annually—equivalent to driving 124,315km. Financially, this could reduce hospital costs by approximately £30,660 per year across five theatres.
While the project has not yet been implemented, ensuring safe introduction and proper approvals is essential. Long-term success will depend on embedding this initiative within broader efforts to reduce theatre energy consumption.
2. Switching from single use to reusable food containers in the main restaurant at RUH, Catering Team
Team members: Fabio Soliman, Georgia-Rose Gleeson, Elizabeth Ray.
Setting / patient group: Catering
Summary
The Royal United Hospitals (RUH) Foundation Trust uses over 4,000 single-use cardboard food containers weekly in its main staff catering outlet, generating significant waste and carbon emissions. To reduce this impact and align with Net Zero goals, the hospital is trialling reusable food containers. Initial testing with a small group of staff showed positive feedback on durability, heat retention, and dishwasher safety. A larger trial with 15 regular customers is underway, with feedback being collected via a questionnaire.
The final project aims to introduce 100 reusable containers per day, encouraging behaviour change and evaluating the feasibility of replacing all single-use containers across hospital catering outlets.
Outcomes
Switching from single-use to reusable meal containers at RUH could save an estimated 1,485 kgCO₂e annually and divert 3,641 kg of waste from landfill. While financial savings are projected at £156.91 per year after the initial investment, additional costs include recycling disposal and a container scanning/payment system.
Collaboration with FSG has been beneficial due to their experience with similar initiatives in other Trusts. The long-term goal is to expand reusable packaging to all meals at Lansdown and phase out single-use cups. Raising awareness about sustainability in catering could encourage behaviour change and openness to future eco-friendly initiatives.
3. Introducing a Patient Group Directive (PGD) for micro-enema use in the radiotherapy outpatient department, Radiotherapy Team
Team members: Sian Griffiths, Consultant Radiographer Urology Specialist; Hazel Clarke, Macmillan Radiotherapy Late Effects Radiographer.
Setting / patient group: Radiotherapy treatment for bladder, prostate or gynaecological cancers.
Summary
Over-prescribing and over-supply of micro-enemas for bowel preparation before radiotherapy lead to medication waste and inefficiencies. This project aims to reduce micro-enema waste by 30% by June 2025 while improving patient experience, reducing financial costs, and easing the workload on prescribers and outpatient pharmacy.
The intervention involves implementing a Patient Group Directive (PGD), allowing patients to receive only the exact number of micro-enemas needed for treatment. This change would streamline prescribing, improve safety by ensuring clinical appropriateness at the point of use, and reduce the time patients spend waiting for prescriptions.
Outcomes
Implementing a Patient Group Directive (PGD) for micro-enemas in radiotherapy could reduce patient time at the hospital and improve prescribing safety by ensuring face-to-face assessments before supply. Environmentally, this change is expected to lower the carbon footprint by 800.83 kgCO₂e annually, equivalent to a petrol car driving 157.7 km.
Financially, reducing unnecessary prescriptions could save £1,353.40 per year, with additional savings from reduced waste disposal. This is the first known study assessing the carbon footprint of micro-enema use in radiotherapy, and once fully implemented, the findings will be shared at conferences and in scientific publications to encourage wider adoption across the UK.
4. Enhancing Sustainability Value in Endoscopy: Simple Switches and PPE Reduction, Endoscopy Team
Team members: Sister Anuska Glendinning-Cranch, Clinical Endoscopist.
Setting / patient group: Endoscopy.
Summary
Endoscopy significantly contributes to healthcare waste, generating around 3.09kg of waste per bed per day. With over 2.1 million procedures performed annually in the UK, making endoscopy more sustainable is essential. A review of procedures led to replacing linen sheets with paper couch roll during transnasal endoscopy (TNE), which quickly expanded to removing unnecessary pillowcases and incontinence pads.
This intervention aims to reduce environmental waste and costs by eliminating off-site linen laundering, reducing hazardous waste disposal, and introducing recyclable tissue paper. Additionally, it promotes sustainability awareness among staff, particularly in PPE usage, to embed long-term sustainable practices in the department.
Outcomes
The changes introduced in endoscopy procedures, such as replacing linen with paper couch roll and removing unnecessary incontinence pads and pillowcases, have minimal impact on patient outcomes, though comfort was assessed through patient interviews. Environmentally, these changes are estimated to save 0.622 kgCO₂e per procedure, totaling 1,747 kgCO₂e annually—the equivalent of driving 5,147 miles or flying London to Glasgow and back 4.7 times.
Financially, full implementation could save £2,160.68 per year. This small-scale intervention highlights how simple changes can drive both environmental and financial benefits while encouraging a broader sustainability mindset across healthcare and beyond.
5. Reducing Waste associated with Infliximab Infusion Bags, Biologics Pharmacy Team
Team members: Rebekah Hewitt, Senior Education & Development Pharmacist/Senior Teacher Practitioner, RUH; Mandy Slatter, Pharmacy Practice Research Lead, RUH; Megan Stevens, Clinical Pharmacy Technician for Biologics/Senior Aseptic Services Technician, RUH; Rebecca Garrett, Rheumatology Senior Sister, RUH; Sean O’Neill, Biologics Day Unit Charge Nurse; Caroline Lock, Specialist Inflammatory Bowel Disease Nurse; Rebecca Pennie, Interim Accountable Pharmacist for Aseptic Services and Radiopharmacy, RUH; Alexandra Bushell, Operational Improvement Manager for Outpatient Transformation, RUH.
Setting / patient group: Biologics Pharmacy.
Summary
Medicines waste is a significant financial and environmental issue, with NHS losses estimated at £300 million annually. This project focuses on reducing waste from high-cost biologic medicine, Infliximab, at the RUH, where 76 infusion bags (373 vials) were discarded in 2023/24, generating 164.85 kgCO₂e per bag. This accounts for 11% of all infliximab bags made on-site.
The aim is to reduce waste by 30% by June 2025. The primary intervention involves improving communication between prescribing clinicians and later-stage teams by creating a Pool on Millenium, ensuring better coordination and reducing unnecessary production and disposal.
Outcomes
Improving communication in infliximab scheduling aims to optimise patient care by ensuring timely treatment while minimising non-clinical delays and unnecessary waste. Streamlining coordination through the Millenium Pool should enhance drug use efficiency and maximise chair space availability. Environmentally, a 30% reduction in wasted infliximab bags (from 76 to 53) could save 3,791.55 kg CO₂e annually—equivalent to driving 11,172 km.
Financially, this would result in annual savings of £6,674. Key success factors include strong multidisciplinary engagement, a structured QI approach, and ongoing mentorship. Formalising system changes and securing leadership support will be essential for sustaining improvements, with potential for wider implementation across aseptic medicines manufacture.