
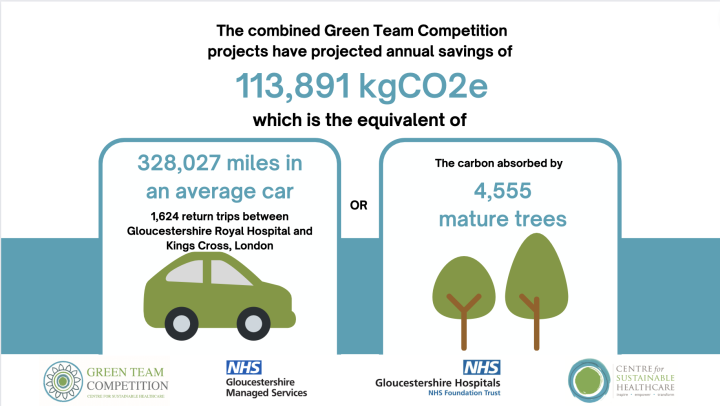
Gloucestershire Hospitals NHS Foundation Trust Green Team Competition expected to save £85,081 and 113,891 kgCO2e annually
The Green Team Competition, which was recently held in partnership with the Gloucestershire Hospitals NHS Foundation Trust (GHFT) and the Centre for Sustainable Healthcare (CSH), has produced remarkable results this year. The competition has generated estimated yearly savings for the Trust of £85,081 and 113,891 kgCO2e, or the carbon footprint equivalent of 328,027 miles driven in an average car (1,624 return trips between Gloucestershire and Kings Cross in London).
In December 2019, Gloucestershire Hospitals was one of the first NHS organisations to declare a Climate Emergency. Committed to benefiting patients, staff, and the surrounding community, the Trust has taken decisive action through its Green Plan. This plan outlines the Trust’s efforts to reduce the impact of climate change on public health and to achieve the NHS’s goal to be carbon neutral by 2040.
Through the Green Team Competition, the Gloucestershire Hospitals NHS Foundation Trust selected six teams to engage in our award-winning, tried and tested leadership and engagement programme. Each team received mentoring from CSH facilitators to drive healthcare transformation through carbon reduction, improved patient care and staff experience, and cost savings.
At the January 31st Judging and Awards Ceremony, the teams presented their projects, including the anticipated savings and opportunities to scale and spread, to an audience from the Trust and the judging panel including:
- Deborah Evans, GHFT Chair
- Deborah Lee, GHFT Chief Executive
- Natasha Parry, Green Council Chair and Sustainability Award Winner
- Rachel Stancliffe, Director at the Centre for Sustainable Healthcare
Read the full Impact Report here.
Green Team Competition Projects
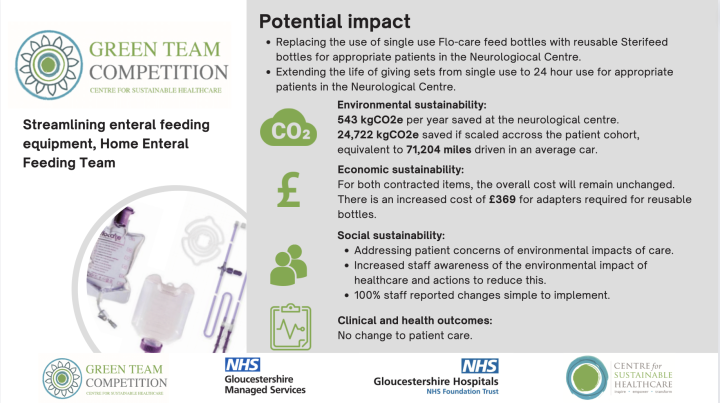
1. Streamlining Enteral Feeding Equipment, Home Enteral Feeding Team (HEFT)
Enterally fed patients in GHFT have expressed concerns to HEFT clinicians about the amount of waste generated by their enteral feeding process. This included cardboard waste, plastic waste-generated by both the feed bottles and the giving sets (the plastic tubing from the bottle of feed to the feeding tube) and fuel emissions produced by their supply deliveries. Responding to these concerns, the HEFT clinicians aimed to find alternative options to improve the patients’ experience.
Team members:
Sarah Williams, Home Enteral Feeding Team Manager (job share) and Dietitian Training Lead; Laura-Marie Baldwin, Advance Home Enteral Feeding Team Dietitian and Adult Team Lead
Method & Impact
The team wanted to evaluate the environmental, financial, social and clinical impacts of replacing the use of single use Flo-care feed bottles with reusable Sterifeed bottles, and extending the life of giving sets from single use to 24-hour use for appropriate patients in the Neurological Centre. They compared the carbon emissions prior to and after changing to re-usable equipment and delayed implementation until old stock was depleted to avoid waste.
The team also educated staff, patients, and relatives on the environmental impact of healthcare and provided training on using and safely cleaning the reusable equipment.
The Neurological Centre was chosen as a pilot site as there are several patients who are eligible to change to the new products. The sample of patients at the centre is representative of the wider population of enterally fed patients within Gloucestershire allowing for the impact of the change to be extrapolated to the entire HEF population and the carbon emissions saving estimated.
There are estimated annual carbon savings of 24,722 kgCO2e, equivalent to driving 71,204 miles driven in an average car, however there was an increased cost of £369 for adapters required for the reusable bottles.
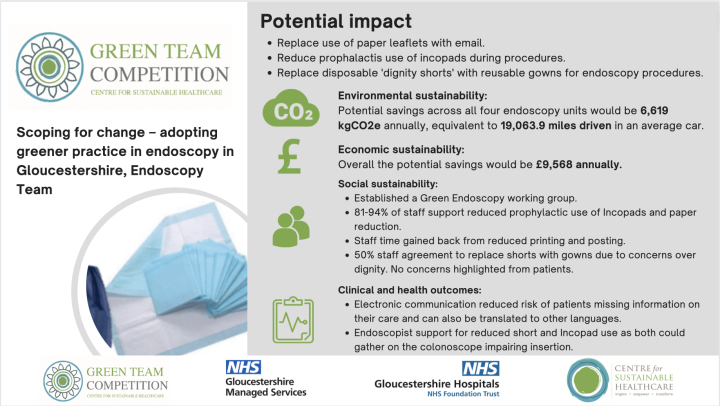
2. Scoping For Change – Adopting Greener Practice in Endoscopy in Gloucestershire, Endoscopy Team
The British Society of Gastroenterology (BSG), Joint Advisory Group (JAG) and CSH recently published a joint consensus on practical measures for environmental sustainability in endoscopy, highlighting that endoscopy is the third largest contributor to NHS carbon emissions due to the high volume of patients and waste generated per procedure.
There is growing enthusiasm nationally for more sustainable practice in endoscopy and the JAG recently recommended that endoscopy services should aspire to develop a green endoscopy working group and initiate at least one environmental initiative. With over 9,000 endoscopic procedures annually across 4 units in Gloucestershire, there is significant potential for carbon savings. Prior to the Green Teams competition, Gloucestershire did not have a dedicated Green Endoscopy working group.
Team members:
Dr Luke Materacki, Consultant Gastroenterologist; Lucy Breach, Endoscopy Sister
Method & Impact
The baseline number of endoscopic procedures performed is recorded monthly. At baseline, all patients would have received a paper leaflet about their procedure, a prophylactic Incopad during flexible-sigmoidoscopy, colonoscopy or gastroscopy and a pair of single use shorts during flexible sigmoidoscopy or colonoscopy. All patients were offered a drink post-procedure which was assumed would utilise one single use cup.
A detailed process mapping exercise was conducted to outline the existing patient pathway in endoscopy and identify areas for change. Three broad aspects of the patient pathway were considered: pre-endoscopy, during the endoscopic procedure and post-endoscopy
- Pre-endoscopy: reducing paper use/postage by offering patients the choice of an electronic copy of their pre-procedure booklet provided via email.
- During endoscopic procedures: reducing single use disposables like shorts, worn by patients for lower GI endoscopy replaced with a washable patient gown. As for prophylactic Incopad use reduction of the ‘just in case’ practice for a more responsive practice such that it would be used if requested by the endoscopist or if high risk of fluid loss was anticipated.
- Post procedure: reducing single use cup use by encouraging patients to bring in their own water bottle or reusable coffee cup. Interestingly some staff felt it was unfair to ask patients to bring their own reusable cup or water bottle, feeling it may increase the stress and anxiety associated with the procedure.
The team estimated annual savings of 6,619 kgCO2e, equivalent to 19,063.9 miles driven in an average car, and £9,568 annually.
3. Orthopaedic Theatres
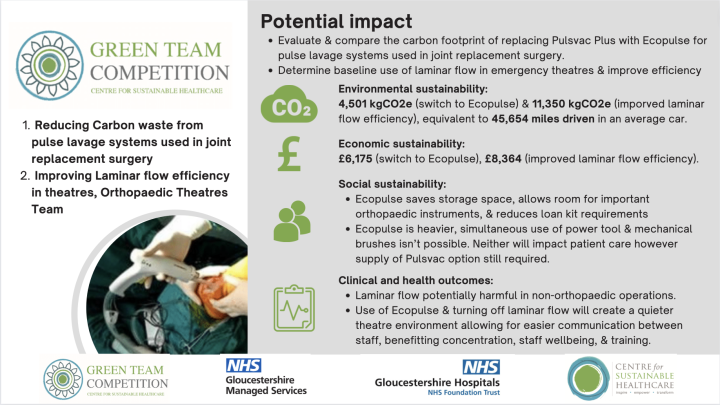
Team 1: Reducing carbon (Co2e) waste from Pulse Lavage Systems used in joint replacement surgery, Orthopaedic Theatres
The Orthopaedic Theatre team perform over 1000 joint replacements per year whilst nationally it is estimated that nearly 440,000 total hip and knee replacements will be performed by 2035. Consequently, thousands of disposable pulsatile lavage systems are used and discarded per year resulting in significant environmental and economic implications.
Pule lavage is used widely in orthopaedic surgery as it plays an important role in modern cementing techniques for total joint arthroplasty by ensuring a clean cancellous bone bed to allow cement inter-digitation. Additionally, it also plays a role in providing high volume washout of soft tissues during wound irrigation. A variety of different disposable pulsatile lavage system are available commercially. These differ mostly in the source of power (battery/AC), plastic/carbon and cost. The current system used at Gloucestershire is the Pulsvac Plus supplied by Zimmer-Biomet® (Warsaw, US). This is a single use, disposable, battery-operated system (8xAA) and is like most of the pulsatile lavage systems used across the UK. The team proposed the use of a novel pulsatile lavage system called the Ecopulse (De Soutter Medical Ltd.®, Aylesbury, UK).
Team members:
Matthew Chan, ST8 Trauma & Orthopaedics Registrar; Amanda Neale, Principal Operating Department Practitioner
Method & Impact
The baseline data was collected using their local National Joint Registry (NJR) report for 2018-2019 (last pre-COVID year) to provide an estimate on their annual knee and hip replacements. The NJR is used by the trust to collect data on all of the total joint replacements performed across the UK. This figure was then used to estimate the annual carbon footprint and cost of each product.
During the clinical implementation and analysis phase, the Ecopulse was trialled using a product evaluation form provided by De Soutter. This trial period was done over a two-week period between 5/9/22 – 23/9/22. The product was used by orthopaedic surgeons and their teams across this period and then an evaluation form was completed. The products were provided by De Soutter free of charge and no funding was required.
The use of Ecopulse has estimated annual savings of 4,629.6 kgCO2e, equivalent to 13,334 miles driven, and savings of £6,175 per year.
Team 2: Improving Laminar Flow Efficiency In Theatres, Orthopaedic Theatres
Laminar flow ventilation systems provide exponential flow of ultra clean air to reduce airborne microbial contamination and subsequent surgical site infection (SSI). Much of the evidence for laminar flow use is based in orthopaedic surgery, especially in relation to prosthetic implantation. This has led to both NICE and BOA advocating for its use in major implant and arthroplasty surgery. However, there is little evidence for the use of laminar flow in other operative indications or surgical specialities. Estimates of the laminar flow use at GHNFT suggests it accounts for up to 30-60% of the overall energy output of our theatres. Consequently, inefficient, and unnecessary use of laminar flow ventilation systems can lead to significant cost and environmental implications.
Team member:
Matthew Chan, ST8 Trauma & Orthopaedics Registrar
Method & Impact
The team assessed the use of laminar flow in orthopaedic and emergency theatres by involving theatre staff and evaluating how the laminar flow is used at GHNFT. The findings showed the laminar flow was used at full power throughout the entire theatre list, in both emergency and orthopaedic theatres.
To estimate the current laminar flow use, details of all the operations performed in August 2022 were reviewed and each case was assessed to see if laminar flow was clinically indicated.
The audit highlighted that only 2 of the 180 cases performed in emergency theatres in August required laminar flow ventilation. This resulted in just over 305 hours of unnecessary laminar flow use. Whilst in orthopaedic theatres around 20% of cases did not require laminar flow amounting to a total of 206 hours of wasted laminar flow use.
By improving laminar flow efficiency, the team anticipates an annual saving of 11,350 kgCO2e (8 -14.7 Tonnes CO2e per year), equivalent to 23,041 – 42,339 miles driven in an average car, and £8,364.
4. Reducing disposable bag use within the Pharmacy Department at Gloucestershire Hospitals NHS Foundation Trust, Pharmacy Team
The Gloucestershire Hospitals NHS Foundation Trust Pharmacy places all their medication supplies to wards, clinics, outpatients, and external sites in individual patient bags, which are then enclosed in another plastic bag for transport. They use a range of LDPE and craft paper bags for different supplies, using thousands of bags annually, generating a carbon footprint of 5,531.56 kgCO2e,(equivalent 16,000 miles driven). The Pharmacy team eliminate bag use for inpatient wards, and reduce outpatient bag use by offering instead of automatically providing them. Transport bags are necessary for safe delivery, but disposable bags could be swapped for reusable ones.
Team members:
Millie Harris, Clinical Pharmacist; Jason Bell, Mental health Lead Pharmacist
Method & Impact
The team analysed the process for dispensing and delivering medications to wards and outpatients, identifying opportunities for improvement. After researching best practices at other hospital pharmacies in the region, the team decided to eliminate the use of disposable bags for inpatient deliveries in phase one.
One project lead also undertook small scale data collection with outpatients, and found that by offering, not automatically providing, bags to outpatients, 2/3rds declined them.
To engage stakeholders, the team raised awareness with pharmacy staff, the Director of Pharmacy, the Divisional Director of Nursing, and informed staff via meetings, emails and posters.
The team conducted their project in two phases:
1. Targeting at an outpatient bag reduction by 30% across both sites
2. Replacement of disposable to re-useable transport bags in the near future
The projects have estimated annual savings of 2,708 kgCO2e, the equivalent of 7,800 miles driven in a car, and £7,500 per year.
5. Reducing the consumption of unnecessary blood samples and idle equipment, Haematology Lab Team
Laboratory sustainability is a difficult challenge due to the requirement for strict quality and infection control procedures. This means running tests with many single use plastic items that must be disposed of to prevent cross-contamination. There is no scalable alternative to single use plastics for items such as gloves, transport bags, pipettes, aliquot tubes, blood tubes and paper blood forms. The use of reagents as part of the testing is also essential to provide assurance that the testing is controlled and accurate.
The team noticed that coagulation tests were sometimes requested inappropriately and that spare citrates were sent and stored without being used. Low value or unnecessary tests increase lab processing time and pressures on lab staff to meet turnaround deadlines, which may in turn impact waiting time for patient results. They also use blood bottles reagents, clinical equipment and disposal bins, all of which is incinerated, unnecessarily.
Finally, the lab's energy consumption is substantial, and the team believed that some equipment could be switched off or put on standby, especially outside of working hours, to improve sustainability and efficiency.
Team members:
Gary Parfitt, Associate Practitioner; Lucy Campbell, Biomedical Scientist; Edward Birt, Medical Lab Assistant; Holly Morgan, Medical Lab Assistant; Tahlima Hussain, Medical Lab Assistant
Method & Impact
The team worked on two different projects.
Project 1: Reducing low value samples sent to the haematology lab from ED
The team spoke to their colleagues to better understand their decision-making processes for coagulation tests and ‘spare’ citrates, with the aim to minimise wasted samples. They looked at all coagulation screens and patient records to obtain data on coagulation screen referrals and reasons given by clinicians for each request. They identified which samples continued to be processed despite being avoidable and other avoidable tests. Lastly, they completed a process map from when spare sodium citrate samples are taken to when they are disposed of in the lab. Based on their findings, they proposed several changes, including:
- Haematology lab staff training for authorising and approving requests, and ED staff training to reduce clinician requests.
- Updating ED protocols/paperwork to raise awareness of wasted first draws, except for winged collection sets.
- Raising awareness to reduce underfilled samples.
- Launching a staff awareness campaign, “Spare a thought for spares”. Or a prompt pop-up message when a clinician requests a spare citrate on sunrise clinical manager e.g. “Only 14% of spare citrates are ever used. Please consider whether you need one”.
The team is collaborating with ED to implement these changes and also working with the Sunrise EPR team to add guidance messages when a spare citrate is requested.
Project 2: Reduce energy usage in (Haematology, Immunology and Boof Transfusion) labs
The team identified that most lab equipment remained on 24/7, even when there were fewer staff and equipment needed in the evenings and overnight. They created a list of all lab equipment and identified opportunities to switch off equipment during idle periods.
The team estimated potential annual savings of 678 kgCO2e from reduced tests/samples, and 62,920 kgCO2e from improving energy efficiency of equipment, quivalent to 183,174 miles driven in an average car. They also estimate potential savings of £846 from reduced tests/samples and £52,924 from improving energy efficiency of equipment.
6. Food Waste Recycling, Gloucestershire Managed Services Team
The UK produced around 9.5 million tonnes of food waste in 2018, which has a significant environmental impact by increasing food production, transportation emissions, and methane and CO2 emissions from landfills.
Unserved food and plate waste (the remaining uneaten food served to patients), is considered food waste in Gloucestershire Royal Hospital and Cheltenham General Hospital. The sites previously wasted 20% of patient meals, equating to approximately 600 meals and £1900 a week across 18 wards. But through various initiatives and engagement with staff, they reduced food waste from wards to 8%.
For their project, the team aimed to minimise the impact of the remaining 8% of food waste. Responsible food waste recycling, can convert waste into fertilisers for agriculture, promoting healthy soil.
Team members:
Marc Thom, Porter Coordinator; Corinne Always, Waste Manager; Neraaj Arora, Assistant Catering Manager; Bridget Hooper, Catering Manager
Method & Impact
The team focused on reducing food waste generated by uneaten patient meals. They found that this stream accounted for a significant portion of their waste. To measure the volume of food waste, the team procured a food scale, trained catering staff on its use, and recorded data on the type of food wasted.
To accommodate recycling, the team made changes to their food waste disposal system. Their recycling process is as followed:
- Food waste would go into biodegradable bags to be weighed.
- A food caddy will be placed in each wards designated waste sluice.
- Ward staff will place food waste into the caddys after each mealtime (3 times daily).
- Food caddys will be collected by portering services after each mealtime (3 times daily) and placed in a designated food waste bin in the hospital waste compound. This bin will be supplied by the food waste recycling company. The food waste recycling company will collect food waste 3 times per week, on a Monday, Wednesday, and Friday, bin quantity can be increased at any time, this will accommodate all the food waste that arrives in the compound. The bins should be clean and fresh after collection (most companies replace old for new), and therefore we should never have rodent/wasp issues.
- They have storage space in the compound for all the bins they would use.
The Trust will be running a pilot scheme for recycling with The Green Block and this will include a trial of food waste recycling. This is scheduled to commence in the new year (2023). Food waste will be taken for anaerobic digestion.
The team anticipates an annual carbon reduction of 393.23 kgCO2e, the equivalent to driving 1,132.6 miles in an average car. Per tonne, Anaerobic Digestion recycling is cheaper, with an estimated annual saving of £72.80.
Awards
 Congratulations to the winning team, the Home Enteral Feeding Team (HEFT) for their innovative project Streamlining Enteral Feeding Equipment, and to the highly commended team, Gloucestershire Mananged Services with their Food Waste Recycling project.
Congratulations to the winning team, the Home Enteral Feeding Team (HEFT) for their innovative project Streamlining Enteral Feeding Equipment, and to the highly commended team, Gloucestershire Mananged Services with their Food Waste Recycling project.
The Centre for Sustainable Healthcare applauds all of the teams that took part in the competition and for their commitment to improving the sustainability of the healthcare system. The competition's outcomes serve as proof of the teams' commitment and efforts, as well as the competition's success in improving clinical practice and advancing sustainability within the healthcare system.

