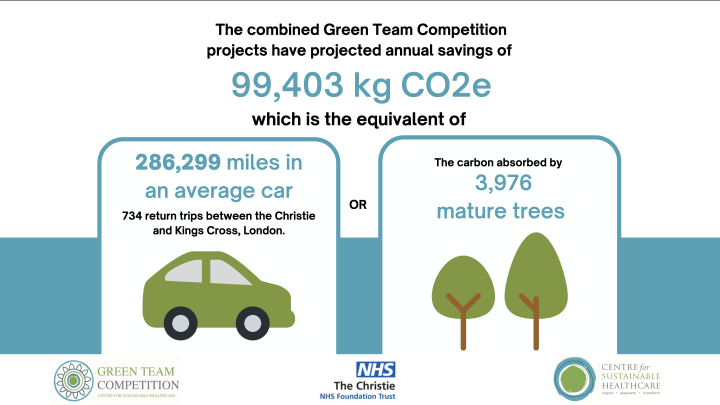
Christie NHS Foundation Trust saves £554,525 and 99,403 kgCO2e with its Green Team Competition
The Centre for Sustainable Healthcare (CSH) is delighted to announce the outstanding results of the Green Team Competition it recently ran with the Christie NHS Foundation Trust. The competition resulted in projected annual savings of £554,525 and 99,403 kgCO2e for the Trust, which is the carbon equivalent of 286,299 miles driven in an average car, or 734 return trips between the Christie and Kings Cross, London.
While healthcare organisations strive to improve the health of populations, their day-to-day operations can contribute to climate change and negatively impact the environment. The National Health Service (NHS) is responsible for an estimated 4% of the country’s carbon footprint, which is roughly equivalent to the emissions profile of Croatia.
The Christie NHS Foundation Trust is committed to reducing its environmental impact and aligning with national goals to become ‘net zero’ by 2040. To achieve this, the Trust has developed a Green Plan which outlines its strategy to reach this target.
Through the Green Team Competition, the Christie NHS Foundation Trust invited five teams to engage in a 10-week project, where they received mentoring from CSH facilitators. The teams were tasked with identifying, developing, running, and measuring the outcomes of sustainable quality improvement projects.
At the January 25th Judging and Awards Ceremony, the teams presented their projects, including the anticipated savings and opportunities to scale and spread. The judging panel consisted of Roger Spencer, Chief Executive, Chris Outram, Chair and Christopher Harrison, Executive Director, from the Christie NHS Foundation Trust, as well as Siobhan Parslow-Williams, QI Education Lead from the Centre for Sustainable Healthcare.
 The Palliative Care team were announced winners of the Christie Green Team Competition, for their innovative project "Photobiomodulation Therapy (PBM): Using Light Therapy for Oral Mucositis”. The Endocrinology team were runners up in the competition with their "Pilot project to assess the impact of identifying patients at high risk of fracture on an acute oncology ward".
The Palliative Care team were announced winners of the Christie Green Team Competition, for their innovative project "Photobiomodulation Therapy (PBM): Using Light Therapy for Oral Mucositis”. The Endocrinology team were runners up in the competition with their "Pilot project to assess the impact of identifying patients at high risk of fracture on an acute oncology ward".
Alex Langstaff, Clinical Nurse Specialist in Supportive and Palliative Care, said "I am so proud to have won this award! If PBM treatment is implemented for our head and neck patients, not only does this get The Christie NHS Foundation Trust closer to the Net Zero Committment, this also significantly improves patient outcomes, alongside savings of over 500k per year!"
The results of the competition are a testament to the dedication and hard work of the participating teams, as well as the effectiveness of the Green Team Competition in transforming clinical practice and promoting sustainability within the healthcare system.
Read the full Impact Report here.
Green Team Competition Projects:
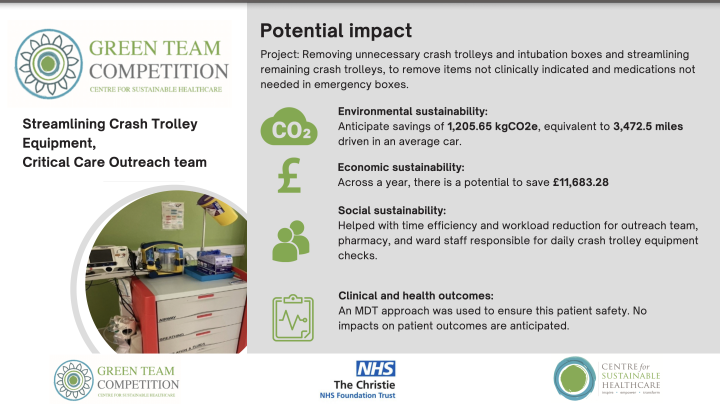
1. Streamlining Crash Trolley Equipment, Outreach Team
It is a Resuscitation Council requirement that healthcare organisations have suitable emergency trolleys with appropriate equipment and medications in the clinical setting. The Critical Care Outreach team are responsible for monitoring and auditing the crash trolleys, of which there are 52 strategically placed around the Christie Trust containing a vast amount of equipment needed for emergencies, vital for patients safety. Through continuously monitoring the crash trolleys, The Christie Outreach Team identified that there may be unnecessary trolleys or items not clinically indicated or required in resuscitation.
Team members
Victoria Croft–Critical, Care Outreach Sister; Jude McLellan–Critical, Care Outreach and AKI Team Lead; Tara Minshall, Resuscitation Equipment Coordinator; Melanie Lowe-Lead, Clinical Pharmacy Technician; Gwendolen Birkett, Senior Clinical Pharmacy Technician
Method & Impact
The team completed a review of all crash trolley locations across the Trust and identified steps to streamline the crash trolleys. They also reviewed locations of their intubation boxes, following an increase in equipment provision through the Covid19 pandemic. The team have successfully removed a duplicate crash trolly, an item not clinically indicated in emergencies (Gelofusin) and medications not needed (Aspirin and Clopidogrel). They have reduced 7 intubation boxes, while ensuring access to equipment in an emergency is not slowed or impacted.
Through these changes to streamline crash trolleys, the team anticipates annual savings of 1,205.65 kgCO2e, equivalent to 3,472.5 miles driven in an average car, and £11,683.28.
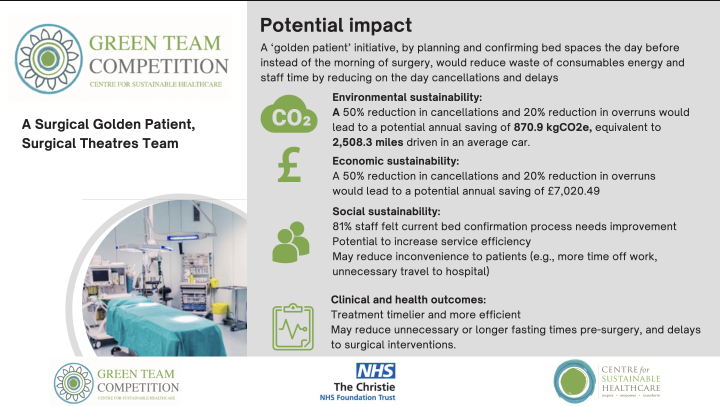
2. A Surgical Golden Patient, Surgical Theatres Team
Operating theatres are a major contributor to the NHS's emissions due to the use of single-use items, anaesthetic drugs and gases, the incineration of waste and packaging, and the large number of healthcare professionals required to safely take care of patients. When a case is cancelled for non-clinical reasons such as bed issues, staff time and many of these items are wasted and disposed of without being used. Bed issues are faced by hospitals across the UK and the Surgical Theatres team looked to identify the potential environmental, financial & social impacts from reducing on the day cancellations and delays due to unconfirmed bedspaces.
Team members
Ana Meastreania, Clinical Education Facilitator for Surgical Theatres; Amy Tabern–Senior Operating Department Practitioner for Anaesthetics & Recovery
Method & Impact
The team identified ‘hotspots’ of waste during delayed or cancelled procedures including equipment, energy, inefficient use of staff time, as well as social and financial costs for patients, staff and the Trust. The process highlighted that the team needed to target a reduction in delays and cancellations in the first place. A ‘golden patient’ initiative, moving bed planning and confirming bed spaces the day before instead of the morning of surgery, would target all the above by reducing on the day cancellations and delays.
The team identified that in the past 12 months, their service has experienced 31 on the day cancellations caused by lack of bed space, equating to 40 hours of theatre overrun time. By implementing a golden patient initiative, the team anticipate a 50% reduction in cancellations and 20% reduction in overrun time would be realistic, and lead to savings of 870.9 kgCO2e, equivalent to 2,508.3 miles driven in an average car and £7,020.49. This saving comes from reduced wasted consumables, reduced staff and patient travel, and energy. The teams long term aim is a 100% reduction in cancellations and delays as a result of bed space issues.
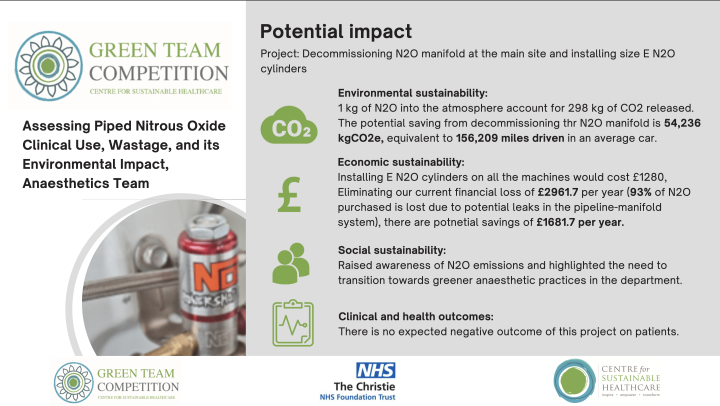
3. Assessing Piped Nitrous Oxide Clinical Use, Wastage and Environmental impact: A Sustainability Quality Improvement Project, Anaesthetics Team
Nitrous oxide (N2O) accounts for at least 80% of the total anaesthetic gas footprint. A recent audit conducted by the NHS Lothian uncovered significant flaws in N2O manifold management, utilisation, and leakage. A key component of reaching Net Zero by 2040 is to explore options to reduce use of anaesthetic gases. However, there was no audit conducted to assess piped N2O related emissions.
The team aimed to assess piped N2O usage and wastage in the anaesthetic clinical practice to identify and explore ways to reduce its environmental (Trust N2O emissions) and financial impact.
Team members
Muhammad Yahya, Specialty and Associate Specialist (SAS) Oncology Critical Care Unit (OCCU) and Anaesthetics; Jonathan Allen, Consultant, OCCU and Anaesthetics
Method & Impact
The team conducted a cross-sectional survey among all full-time independent anaesthetic practitioners, including consultant anaesthetists and SAS anaesthetists, to assess the use of N2O in anaesthetic clinical practice. They also conducted a technical survey, collecting data from the estate, pharmacy and the theatre and anaesthetic machine. Based on their findings, the following recommendations were made to the anaesthetic department:
- Decommission N2O manifold at the main site which consumes approximately 70% of the N2O with no clinical benefit.
- Keep portable N2O cylinders to be made available to use when required.
By installing size E N2O cylinders, and decommissioning N2O manifolds at the main site, there are potential annual savings of 54,236 kg CO2e and £1681.7.
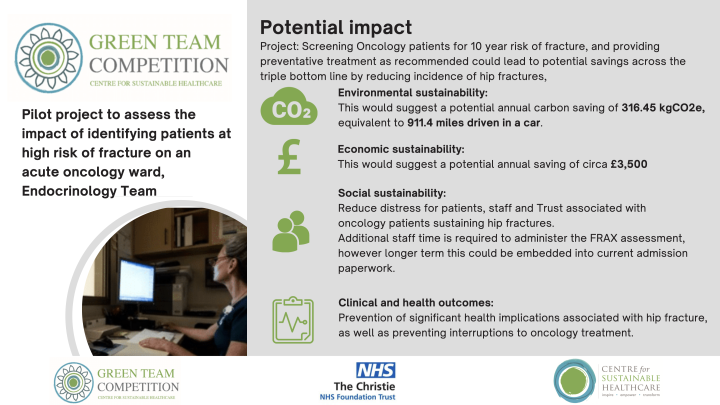
4. Pilot project to assess the impact of identifying patients at high risk of fracture on an acute oncology ward, Endocrinology Team
Patients with an oncology diagnosis are likely to be at higher risk of fragility fracture for several reasons. There is a lack of local and national guidance on bone protection in adult oncology patients. The FRAX assessment tool was developed to evaluate fracture risk of patients, providing a ten-year assessment of potential major fracture and can be used to identify patients at risk.
The team aimed to review the fracture risk in an unselected group of Oncology in-patients using the FRAX questionnaire and determining the workforce/environmental/medication implications of this. Environmental and financial cost of screening and subsequent treatments was compared to the impact of a fracture and its management.
Team members
Tom Hicklin, Ward Manager Ward 11; Claire Higham, Consultant Endocrinologist; Mohitraje Mankumare ,IMT-2 Trainee
Method & Impact
A modified FRAX questionnaire was administered to patients and the outcomes were evaluated for their workforce, economic and environmental outcomes and compared to the environmental impact of a hip fracture.
There are various interventional treatment options, however for the purposes of the teams' audit, the treatment chosen was Adcal. The team estimated that for 100 patients treated, they could prevent 1 fracture per year, which is a project annual saving of 316.45kgCO2e and £3,500.
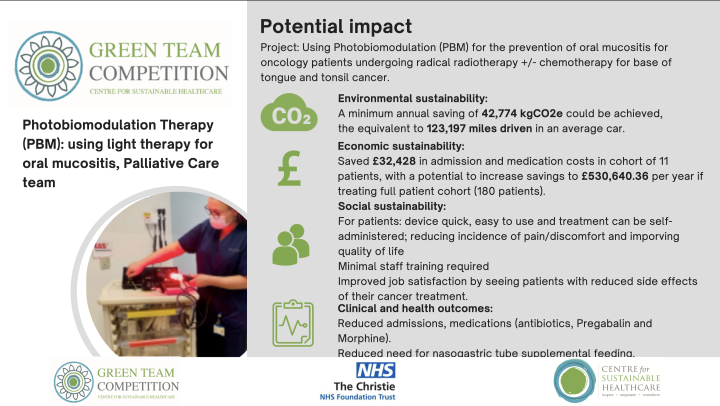
5. Photobiomodulation Therapy (Pbm): Using Light Therapy For Oral Mucositis, Palliative Care Team
The Christie NHS Foundation Trust in Manchester is one of the largest cancer treatment centres of its type in Europe. When diagnosed with head and neck cancer, many patients require radical treatment inclusive of both chemotherapy and an extensive course of radiotherapy. The most problematic of early side effects for patients with a cancer diagnosis involving base of tongue and tonsil canceris mucositis; inflammation and breakdown of the mucosal lining in the oral cavity/oesophagus5.
The National Institute for Health and Care Excellence (NICE) published interventional procedures guidance recommending the use of Photobiomodulation (PBM) for the prevention or treatment of oral mucositis. PBM involves application of light to tissues to promote healing, reduce inflammation and increase cellmetabolism. PBM stimulates the natural healing process, in turn reducing pain and improve the quality of life of our head and neck patients.
The team aimed to evaluate the clinical, social, financial and environmental impacts of PBM as a supplemental treatment for the prevention and/or reduction of oral mucositis for base of tongue and tonsil oncology patients undergoing radical radiotherapy +/- chemotherapy.
Team member
Alexandra Langstaff, Clinical Nurse Specialist, Supportive and Palliative Care
Method & Impact
Over a period of four months a PBM unit was sourced and tested in a small cohort of the team’s head and neck patients to evaluate if PBM would be an effective treatment for reducing mucositis symptoms alongside the associated treatments and admissions.
A total of twenty-two patients were included with an equal number of patients in the control group and study/treatment group, both of which had a comparable mean age and were undergoing radical radiotherapy +/-chemotherapy for base of tongue or tonsil cancer.
The control group completed radiotherapy and did not receive PBM treatment. They were treated for symptoms of mucositis as they presented.
The treatment group received the same radiotherapy treatment as the control group, but they also received PBM treatment before each radiotherapy session for 30 consecutive days (the common duration or a radiotherapy treatment regime).
The team compared across the control and treatments groups, the severity of mucositis symptoms, frequency and length of unplanned admissions, type and dose of medications required because of mucositis for pain, and any further treatments or interventions required because of mucositis.
Based on treatment eligibility to the full 180 tonsil and base of tongue cancer patients per year, having one 30-day course of radiotherapy and PBM a year, their projected savings are 42,774 kgCO2e and £530,640.36 per year in admission and medication costs.
Patients also felt involved in their treatment and reported they felt ‘empowered’ and in control in a time where loss of control has been felt throughout. “It was easy to use and I would recommend it to others undergoing head and neck radiation”.
The Centre for Sustainable Healthcare congratulates all the teams who participated and thanks them for their hard work and dedication to making the healthcare system more sustainable.
We would like to extend a special thank you to William Blair - Sustainability Manager, Joanne Woolley - Clinical audit and improvement manager and Angela Hayes - Clinical Nurse Specialist in Supportive and Palliative Care, informal role in Clinical Sustainability, for commissioning the competition, partnering with us and for wholeheartedly working to support and mentor teams. We also encourage other healthcare organisations to follow the example of the Christie NHS Foundation Trust and find ways to implement sustainable practices in their own organisations.