The Desflurane Reduction Project
Anaesthesia is the speciality responsible for patient care before, during and after operations. During the operation, the type of anaesthetic delivered can vary depending upon the clinician’s preference and suitability for the patient. Patients can undergo traditional general anaesthesia using anaesthetic gases or intravenous drugs to put them to sleep. Alternatively, patients can be kept awake but comfortable and safe for their operation using regional anaesthetic techniques: epidural or spinal injections, or limb blocks.
Anaesthesia as a speciality contributes up to 2% of the NHS carbon footprint or 5% of an acute hospital’s carbon footprint. The predominant source of this footprint is from anaesthetic gases, used during traditional general anaesthesia. The most harmful of these include Nitrous Oxide and Desflurane.
The harm produced by these gases on the environment is described by their Global Warming Potential (GWP). Its value describes the amount of heat trapped over a 100 year period within the atmosphere, compared with the similar mass of carbon dioxide (CO2) - CO2 has a GWP of 1.
Of the commonly used anaesthetic agents in circulation, the table below provides reference of their GWP’s.
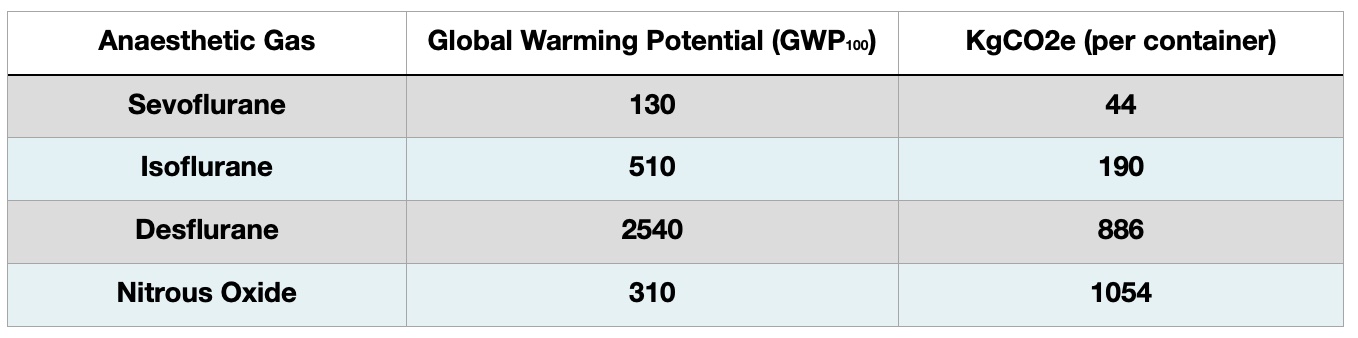
Because of the large volume used, Nitrous Oxide is the most harmful. In fact, it turns out that a large proportion of the Nitrous Oxide ‘used’ in operating theatres is actually wasted (learn more about the Nitrous Oxide Project here).
There has been excellent work done around the country to mitigate the use of both Nitrous Oxide and Desflurane. Although Desflurane usage has fallen as a result, it is such a potent greenhouse gas that any usage has a significant climate impact. A number of clinicians continue to use Desflurane, arguing that it is clinically superior to other commonly available anaesthetic agents in some situations. National usage of Desflurane can be monitored through the Model Health System tool. Access can be acquired for anyone with a nhs.net email account.
Why is Desflurane Bad for the Environment?
Desflurane is 2540 times more potent as a greenhouse gas than an equivalent mass of Carbon Dioxide. A 240mL bottle of Desflurane, completely vaporised will produce the equivalent of 886kg of carbon Dioxide. In everyday terms, this is the equivalent of driving 3072 miles from London to Naples and back, in a petrol engine car.
The video below discusses the clinical, environmental, social and financial impacts of Desflurane use.
What are the Clinical Indications for and Impacts of Desflurane use?
Desflurane is a known bronchoconstrictor, particularly at the beginning of surgery and at higher MAC’s, resulting in poor ventilatory function. This is exacerbated in the obese cohort for whom ventilation is already more challenging. Its faster onset and offset provides no clinical benefit. Despite having a faster offset, or faster wake up time, the rates of respiratory complications associated with Desflurane use have been found to be higher than Sevoflurane. Other anaesthetic gases can achieve similar offset times as Desflurane when gases are titrated down towards the end of surgery, which may be safely done through the use of BIS monitoring. End organ perfusion, focusing on liver and renal function, shows no beneficial outcomes with the use of Desflurane when compared to other agents. Volatiles in comparison to propofol are arrythmogenic. There are similar findings with Desflurane and Sevoflurane use during neuro-surgery. Despite the apparent faster wake up times in theatres, cognitive recovery rates after 30 minutes between volatile agents are similar and there is no clinically significant reduction in time spent in recovery.
The Economic Implications of Desflurane
We have already considered the environmental harm created by Desflurane, but, the economic costs of Desflurane use are higher than the next anaesthetic agent commonly used - Sevoflurane. Desflurane requires 3x more volume to deliver the same clinical effect as Sevoflurane. For every £1 spent on Sevoflurane you would have to spend £4.49 on Desflurane to get the same clinical effect (prices are for the Freeman Hospital 2020/2021).
In summary, there is no clinical indication to continue using Desflurane and, given it is the most expensive and environmentally harmful volatile in use, it does not belong in any theatre.
Sevoflurane is the next obvious choice if using a volatile agent. Other options include total intravenous anaesthetic (TIVA), however, the non-carbon environmental harms of TIVA are unclear and are still to be explored.
But, do we need to give a general anaesthetic?
How to reduce Desflurane use in your hospital
- If you are a trainee, develop links with consultants who share a similar interest. Regional networks can help establish these links.
- With your consultant, or if you are the consultant, liaise with your trust sustainability team. They will be interested in reducing Desflurane use as much as you! They may already know how much Desflurane is being used in your hospital, annually.
- Audit how much Desflurane is currently being used if the sustainability team do not have the information. This can be done one of two ways:
- Talk to the clinical pharmacist who has access to purchase records and establish how much Desflurane is purchased on a monthly basis.
- Do a rolling audit of anaesthetic gas use by logging Desflurane use from the ventilator at the end of each shift (best done in a team as nights tend to be the best time to log data).
- Do a survey to understand the culture of current Desflurane use in your department.
- Once you have your baseline information, you can present your findings locally.
- If you feel it will change departmental attitudes around Desflurane, I am happy for you to share my video.
- Once you’ve delivered your presentation, repeat your baseline audit to show if you’ve changed departmental culture.
- If there has been a unanimous decision to remove Desflurane use then:
- Firstly, well done!
- Contact pharmacy to ensure no further Desflurane is purchased.
- Liaise with estates to siphon off safely any Desflurane remaining in the vaporisers.
- Inform theatre anaesthetic assistants that no one should be asking for Desflurane.
- Repeat the audit after a couple of months to demonstrate a statistical difference through your interventions.
Can Desflurane Reduction be Successful?
Desflurane reduction at the Freeman Hospital, in Newcastle Upon Tyne followed the above approach. Answering the question of whether there was any clinical indication for ongoing Desflurane use overcame the final barrier. In December 2021 we went Desflurane free!
There was some apprehension to its removal but overall, the clinicians who commonly used Desflurane easily adapted to using other anaesthetic agents available. A repeat audit in January 2023 demonstrated there was no use or further purchasing of Desflurane by pharmacy throughout 2022. Remaining stock has been stored away until there is a consensus by Greener NHS as to how to safely manage this excess. This remaining stock cannot be used as the vaporisers have been removed from theatre suites.
This project has successfully shown everyone has the capability to deliver sustainable change.
Project Lead
Jason Gandhi
Association of Anaesthetists and Centre for Sustainable Healthcare National Fellow in Environmentally Sustainable Anaesthesia, Newcastle University Teaching Hospitals. envirofellow@anaesthetists.org
Acknowledgements
Dr Ian Baxter, the Anaesthetic department at Freeman Hospital and the Sustainability Team at Newcastle University Teaching Hospitals.
The team at the Centre for Sustainable Healthcare

