
Introducing team 2 of the Green Surgery Challenge
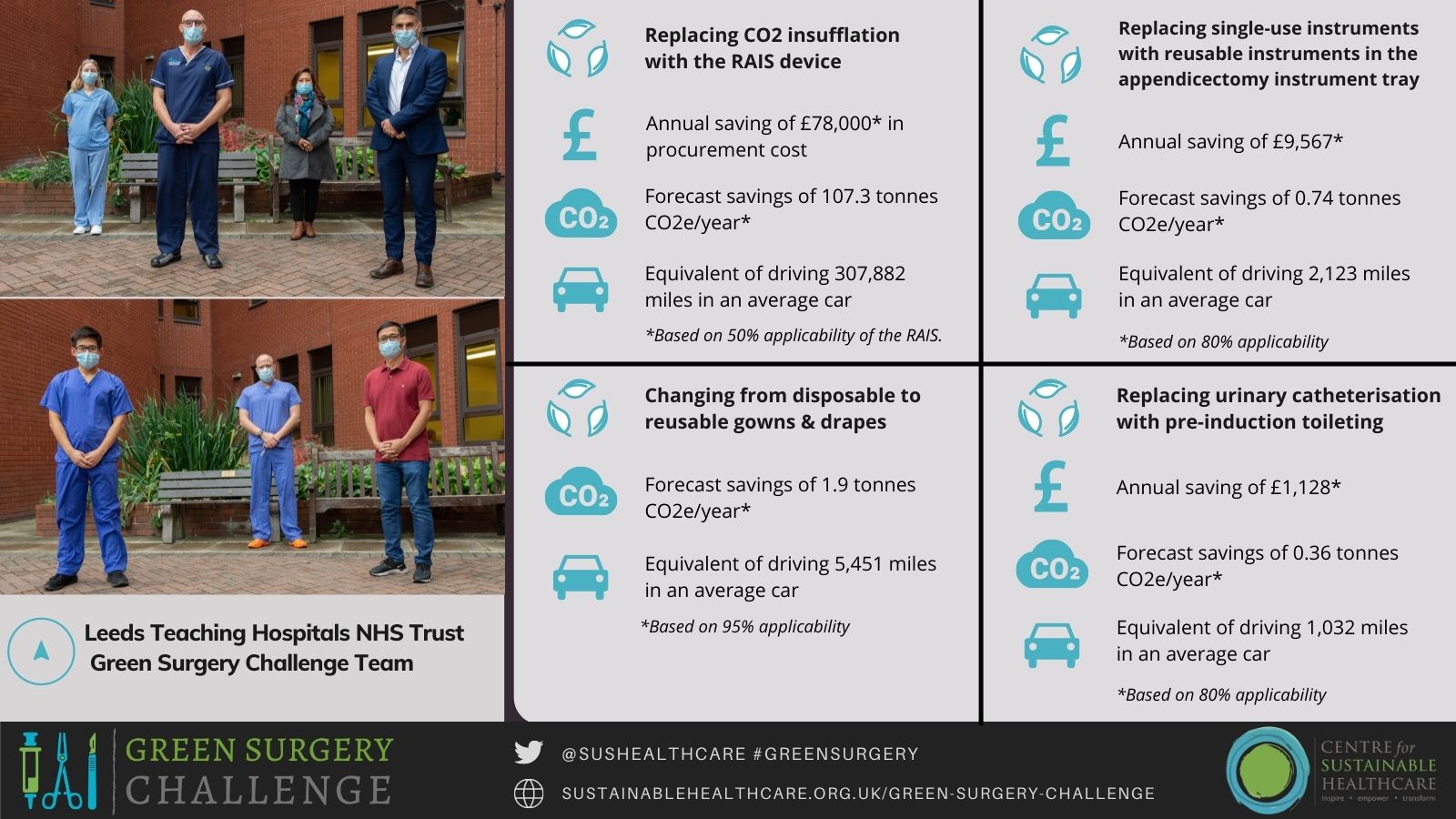
The Leeds Teaching Hospital NHS Trust team's Green Surgery Challenge project included four components:
- Replacing CO2 insufflation with the RAIS device
- Changing from disposable to reusable gowns and drapes
- Replacing urinary catheterisation with pre-induction toileting
- Replacing single-use instruments with reusable instruments in the instrument tray for appendicectomy
These approaches are examples of the third and fourth principles of sustainable clinical practice, ‘lean’ service delivery and low carbon alternatives to existing practices.
The team was led by Mr Adam Peckham-Cooper, Consultant Emergency General Surgeon and Honorary Senior Lecturer, Mr Aaron Quyn, Consultant General Surgeon, Associate Clinical Professor of Surgery, Deputy Director NIHR Surgical MedTech Co-operative. The project team included Mr Noel Aruparayil, General Surgery Specialist Registrar, Honorary Research Fellow, Global Health Research Group-Surgical Technologies, Mr Thomas Pike, General Surgery Specialist Registrar, NIHR Clinical Lecturer, Dr Katie Boag, Emergency General Surgery Clinical Fellow, Dr Peter Culmer, Associate Professor in Healthcare Technologies, Engineering Lead NIHR Global Health Research Group-Surgical Technologies and Mr Tim Ho, Medical Student.
Read the full case study here.
Summary
Medical gases, energy use and consumables are significant contributors to the carbon footprint of surgical procedures. The team decided to focus on laparoscopic appendicectomy as a particularly resource-intensive procedure that is performed frequently; in the United Kingdom, acute appendicitis has an incidence of 7-12% and is the most common abdominal surgical emergency, resulting in 42,000 appendectomies per year.
The team carried out their project using the Sustainable Quality Improvement (SusQI) framework. A holistic review of the laparoscopic appendicectomy process using a process map revealed numerous opportunities to reduce the environmental impact. The team implemented two key changes, modelled the third change, and made plans for further improvements.
The team listed all the instruments in the current procedure packs and were able to reduce these from 119 to 49, both reducing the number of trays of surgical instruments requiring sterilization and the number of single-use items opened but not used. These ‘Green Trays’ are now begin used routinely.
Patients are now also routinely being asked to pass urine before entering the anesthetic room to eliminate the need for urinary catheterization, reducing the use of consumables and potentially improving the patient experience.
The team also modelled the change in resource use by using a gasless procedure for laparoscopic appendicectomy by carrying out a real-time cadaveric study, simulating the innovative surgical procedure. The Leeds Global Health Research Group has developed a new device, RAIS (Retractor for Abdominal Insufflation-less Surgery) that mechanically creates a space within the abdomen to allow surgery to be carried out, rather than using insufflated gas. The procedure was modelled using the standard procedure packs and the green tray, as well as further changes such as re-usable drapes and gowns.
All these interventions were shown to both reduce the environmental impact of the procedure and reduce cost. Medical gas use was a surprisingly large contributor to the overall carbon footprint of the procedure. From a global perspective the team think that the RAIS device would expand global surgical access (where access to medical gases is scarce and funds for consumables severely constrained) and contribute significantly towards the UN Sustainable Development Goals (25). Working with surgeons in low- and middle-income countries also provides an opportunity for reverse innovation, improving sustainable surgical practice in the UK.
Carbon and Financial Impact
- Replacing CO2 insufflation with the RAIS device has forecast savings of £78,000 in procurement costs alone and 107.3 tonnes CO2e/year (based on 50% applicability of the RAIS). This is the same amount of CO2e as driving 307,882 miles* in an average car.
- Changing from disposable to reusable gowns and drapes has forecast savings of 1.9 tonnes CO2e/year (based on 95% applicability). This is the same amount of CO2e as driving 5,451 miles* in an average car.
- Replacing urinary catheterisation with pre-induction toileting has forecast savings of £1128 in costs and 0.36 tonnes CO2e/year (based on 80% applicability). This is the same amount of CO2e as driving 1,032 miles* in an average car.
- Replacing single-use instruments with reusable instruments in the instrument tray for appendicectomy has forecast savings of £9,567 in costs abd 0.74 tonnes CO2e/year (based on 80% applicability). This is the same amount of CO2e as driving 2,123 miles* in an average car.
In total, these projects have a forecast annual saving of £88,695 and 110.3 tonnes CO2e! This is the carbon equivalent of driving 316,488 miles* in an average car (552 times from G7 to COP26).
*CO2e comparison: Distance from G7 (Carbis Bay, Cornwall) to COP26 (Glasgow): 573 miles / 922 km. Average car (unknown fuel) GHG emissions: 0.34851kgCO2e/mile.
Dr Olivia Bush, Programme Lead for Sustainable Clinical Practice at the Centre for Sustainable Healthcare, said:
“Our current knowledge suggest that to reduce environmental impact and improve overall sustainable value both implementation of existing solutions and innovation will be required; both innovation of clinical pathways guided by the principles of sustainable practice and entirely novel approaches, devices and technology. The team addressed both aspects of innovation through meticulous process mapping to identify impactful process changes and modelling of the use of this team’s novel device.”
The Green Surgery Challenge is a special adaptation for clinical specialties of the Centre for Sustainable Healthcare’s flagship programme, the Green Ward Competition (an award-winning clinical leadership and engagement programme to improve the environmental sustainability of healthcare). The challenge has been created and delivered through collaboration with a group of supportive partners including NIHR MedTech Co-operative in Surgical Technologies, Royal College of Surgeons England, Royal College of Surgeons Edinburgh, The Sustainable Healthcare Coalition, Brighton and Sussex Medical School and the Association for Perioperative Practice. The Challenge has been made possible through the generosity of our Gold Funders and Sponsors NIHR MedTech Co-operative in Surgical Technologies and Elemental Healthcare, Silver Sponsors Royal College of Surgeons England and Royal College of Surgeons Edinburgh, Bronze Sponsors the AHSN Network, Vanguard Medical Remanufacturing, and Bowa Medical UK. For more information, please click here.

