
Introducing team 5 of the Green Surgery Challenge
We are pleased to introduce the team from Imperial College Healthcare NHS Trust who will be joining the Green Surgery Conference November 4th as one of the Green Surgery Challenge finalists.
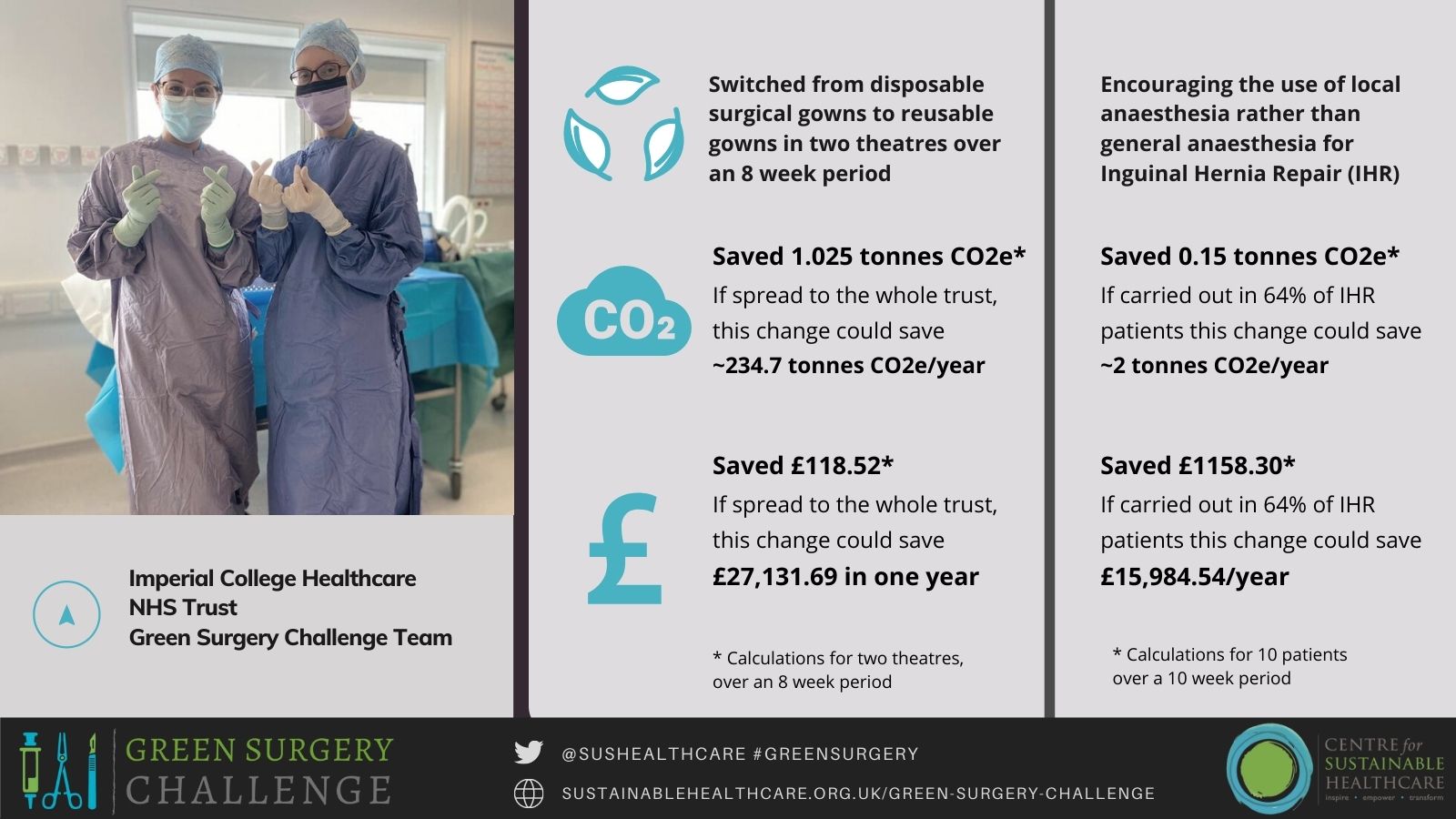
The team selected two areas to work on as part of the Green Surgery Challenge; tackling the use of anaesthetic gases by encouraging the use of local anesthesia (LA) with/without sedation for inguinal hernia repair (IHR) instead of general anaesthesia (GA) and reducing the use of single-use consumables by switching from disposable sterile surgical gowns to reusable surgical gowns. These approaches are examples of the third and fourth principles of sustainable clinical practice, ‘lean’ service delivery and low carbon alternatives to existing practices, whilst also reducing operational resource use.
The project was co-led by Surgical Registrars and Clinical Research Fellows Jasmine Winter-Beatty and Jonathan Gan. Members of the team were Henry Robb, Surgical Core Trainee, Simon Dryden, Clinical Research Fellow, Institute of Global Health Innovation, Patricia Ortega, Bariatric Surgery Fellow, Tabetha Granger, Surgical Core Trainee, Ben Russell, Foundation Year 1 doctor, Sanjay Purkayastha, Consultant Bariatric Surgeon and Senior Clinical lecturer. Mike Kynoch, Anaesthetic Consultant, gave specialist advice to the team on anaesthetic practice.
Read the full case study report here.
Summary
The team carried out their projects using the Sustainable Quality Improvement (SusQI) framework including assessing outcomes against the elements of ‘sustainable value’, clinical outcomes for the patient and population, environmental impact, social impact and financial resource use.
1) Increasing use of LA (+/- Sedation) instead of GA for open IHR where patients were eligible:
The team identified IHR surgery performed under GA as a potential carbon hotspot in the NHS due to the use of anaesthetic gases, which are also greenhouse gases. Anesthetic gases are responsible for 42% of carbon emissions related to the surgical procedure. Switching to the use of LA could result in considerable reductions in carbon emissions, with indirect health benefits for the whole population. Additionally, IHR performed under LA may result in improved patient outcomes, financial savings, and a quicker return to daily life and work due to a reduced length of stay (LOS) in hospital.
The team checked national guidelines for assessing patients’ eligibility to undergo IHR under LA. The team then discussed the guidance and the benefits of carrying out surgery for IHR under LA with surgical and anesthetic colleagues. Eligible patients were identified by prospectively screening surgical lists, speaking to the consultant responsible for their care to agree eligibility, and then calling patients to offer them the procedure under LA, rather than the GA that they had been listed for originally.
- Clinical outcomes were compared for the groups of patients undergoing inguinal hernia repair under general and local anaesthetic.
- Environmental impacts of the change were calculated by auditing how many IHR were carried out under GA vs LA. The team then audited the usage of drugs, equipment, anaesthetic agents, and energy use in the patient pathway from anaesthetic induction through to discharge for carrying out IHR under GA and LA; this allowed them to calculate and compare the carbon footprint for the two anaesthetic approaches.
- Financial impact was determined by calculating the cost of pharmaceuticals, equipment, anaesthetic agents, and energy use, as well as the accompanying financial expenditures for carrying out IHR under GA and LA so that a comparison could be made. Additionally, the team compared the average length of hospital stay for IHR under LA and GA, as well as the associated costs to the trust using pre-pandemic 2019 data.
- Simon Dryden led on evaluating Social Impact by devising and conducting patient surveys on the amount of time patients and their caregivers took off from work, any additional income lost due to the hospital stay, and impacts on activities of daily living.
2) Replacing disposable surgical gowns with reusable gowns
Switching from disposable surgical gowns to reusable gowns has the potential to decrease pollution and the production of carbon emissions, and is a way to allow staff to carry out their work in line with sustainability values that are important to most healthcare professionals (this can contribute to improved staff morale) and generate financial savings associated with reduced resource use, waste disposal and transport.
Samples of reusable surgical gowns were procured and made available for theatre staff to use.
- Clinical outcomes: gowns met safety standards for medical use.
- Environmental impact: the team used 2019 procurement data from the Trust and calculated the projected environmental impacts of switching to reusable gowns based on data from peer-reviewed studies.
- Financial impact was determined with assistance from the procurement department who provided the team with key metrics regarding the financial cost of the trust's current reusable gowns. The suppliers of the team's current reusable gowns provided a cost per use estimate for the reusable gowns, which included waste disposal and transportation.
- Social impact was determined by distributing surveys to staff to assess their use of reusable gowns. The team supplemented the survey with face-to-face interviews with surgeons, anesthetists and nurses who had tried out the reusable gown samples.
Carbon and Financial Impact
Both interventions resulted in significant gains in sustainable value, with environmental and financial benefits. During the project period, the projects saved 1.175 tonnes CO2e and £1,276.82, which leads to a forecast annual saving of approximately 8.5 tonnes CO2e/year and £16,740. If the reusable gowns were spread to the whole trust, it could save 234.7 tonnes CO2e over a year.
Additionally, the team are communicating their findings at events within their Trust and have already noticed an increase in awareness of sustainable healthcare practice and cultural change towards prioritizing low carbon care within the organisation.
Dr Olivia Bush, Programme Lead for Sustainable Clinical Practice at the Centre for Sustainable Healthcare, said:
“Under Jasmine Winter-Beatty’s and Jonathan Gan’s leadership this team achieved a huge amount, modelling the impact of two change projects and meticulously collecting of data to provide an accurate carbon footprint of the change from general to local anaesthesia, which was possible due to their strong relationship with their anaesthetic colleagues. They also managed to achieve a change in practice, which has been more than usually challenging due to the pandemic, and are working on embedding one of their successful changes.”
The Green Surgery Challenge is a special adaptation for clinical specialties of the Centre for Sustainable Healthcare’s flagship programme, the Green Ward Competition (an award-winning clinical leadership and engagement programme to improve the environmental sustainability of healthcare). The challenge has been created and delivered through collaboration with a group of supportive partners including NIHR MedTech Co-operative in Surgical Technologies, Royal College of Surgeons England, Royal College of Surgeons Edinburgh, The Sustainable Healthcare Coalition, Brighton and Sussex Medical School and the Association for Perioperative Practice. The Challenge has been made possible through the generosity of our Gold Funders and Sponsors NIHR MedTech Co-operative in Surgical Technologies and Elemental Healthcare, Silver Sponsors Royal College of Surgeons England and Royal College of Surgeons Edinburgh, Bronze Sponsors the AHSN Network, Vanguard Medical Remanufacturing, and Bowa Medical UK. For more information, please click here.

