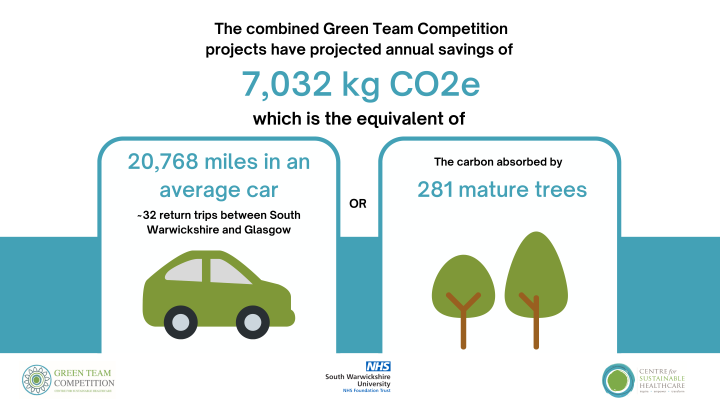
South Warwickshire University NHS Foundation Trust Green Team Competition expected to save £116,194 and 7,032 kgCO2e annually
In May of this year, South Warwickshire University NHS Foundation Trust commenced a Green Team Competition in partnership with the Centre for Sustainable Healthcare. The competition has brought anticipated annual savings to the Trust of £116,194 and 7,032 kgCO2e. This is the carbon footprint equivalent of driving 20,768 miles in an average car (or 32 return trips between South Warwickshire and Glasgow).
South Warwickshire NHS Foundation Trust made a commitment in April 2022 to achieve net zero carbon emissions by 2040. Statement to this, is the work commenced in April 2023 to decarbonise Warwick Hospital estates through a £9.2M investment which will bring a reduction in carbon emissions of circa 800 Tonnes per annum. However, South Warwickshire recognise that changes to how care is provided are also needed to meet net zero targets and so the Green Team Competition was commissioned.
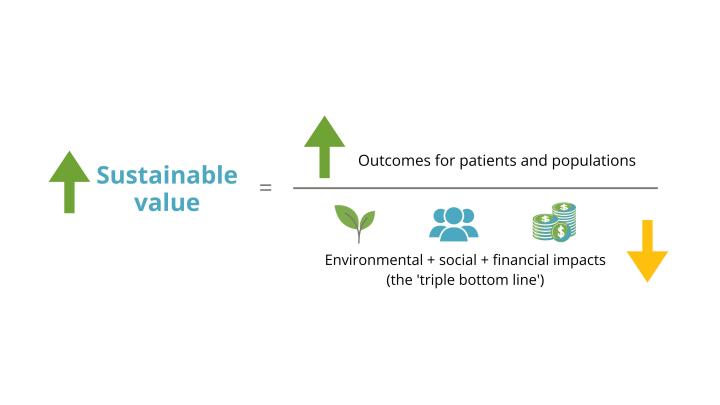
Through the Green Team Competition, six teams from South Warwickshire University NHS Foundation Trust were selected to engage in our award-winning programme in sustainability in quality improvement (SusQI) that transforms expert knowledge into action. Each team received mentoring from CSH facilitators to drive healthcare transformation by developing, implementing and measuring the impact of projects through the lens of the sustainable value equation.
SWFT have also engaged five staff members from sustainability, project officer and improvement teams to engage in the CSH SusQI Academy. The Academy members have supported Green Teams through the competition process, and as part of their Academy work as exploring how to embed sustainability into quality improvement widely across the Trust.
At the September 29th Showcase and Awards Ceremony, the teams presented their projects, including the anticipated savings and opportunities to scale and spread, to an audience from the Trust and the judging panel including:
- Charles Ashton, Medical Director, SWFT
- Sophie Gilkes, Chief Strategy Officer, SWFT
- Siobhan Parslow Williams, QI Education Lead, Centre for Sustainable Healthcare (CSH)
Green Team Competition Projects
Read the full Impact Report here or view the project summaries below.
- Reducing routine blood testing, Frailty and Care of the Elderly Wards team
- Lean pathway and low carbon alternatives in curette and cautery skin surgery, Dermatology team
- Reducing Continence products waste, Neuro rehab team
- Improving the environmental impact of patients with diabetes and on insulin, Diabetes team
- Effect of reducing physiotherapy referrals from care homes on waiting lists through health promotion, physical activity, and falls prevention, Physiotherapy team
- Reducing Wastage in the Medicines Pathway, Pharmacy team
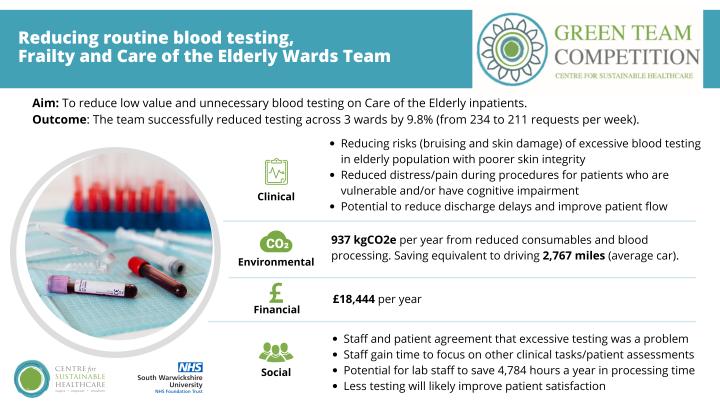
1. Reducing routine blood testing in Frailty and Care of the Elderly Wards.
Summary: Many elderly inpatients are subject to regular (up to daily) blood tests during their inpatient stay to help monitor their condition and guide their treatment. However, overuse of testing is commonplace in this population of patients which can negatively impact multiple aspects of the process and decrease patient satisfaction.
Team members: Ellie Berry, Advanced Clinical Practitioner (Frailty) - Project Lead; Lorna Bannan, Assistant Service Manager – Care of the Elderly & Frailty
Aim: Reduce low value and unnecessary blood testing on Care of the Elderly inpatients.
Method & Impact
The team developed a new decision-making tool to aid clinicians in deciding if blood testing was necessary at all, and if so, which tests were necessary for each patient to guide their treatment. The team promoted the tool and clinical behaviour change via a comms campaign and presentations to staff. They also presented to wider staff at a Trust event. 100% of staff surveyed prior to the project launch felt that too many blood tests were taken on our patient group and that this process is wasteful.
Before the intervention, 234 phlebotomist request forms (with an average of 4.2 tests per form) were submitted in a 7-day period across 6 wards. After the intervention, this reduced to 211 phlebotomist request forms (with an average of 4 tests per form). This is a 9.8% reduction in requests.
Projected across a year, the team anticipate savings of £18,444 and 937 kgCO2e per year, equivalent to driving 2,767 miles in an average car. Ward, phlebotomy and lab staff will all gain back time to redirect to higher value work, with a potential for lab staff to save 4,784 hours per year in blood processing time from 6 wards alone! The project will also being clinical and social benefits to patients, helping to reduce bruising and skin damage to the elderly population who often have vulnerable skin tissue and to reduce pain and distress for patients with cognitive impairment who may not fully understand the need for repeated blood tests. While it was not possible to measure in the competition timeframe, reduction in testing also has the potential to reduce discharge delays.
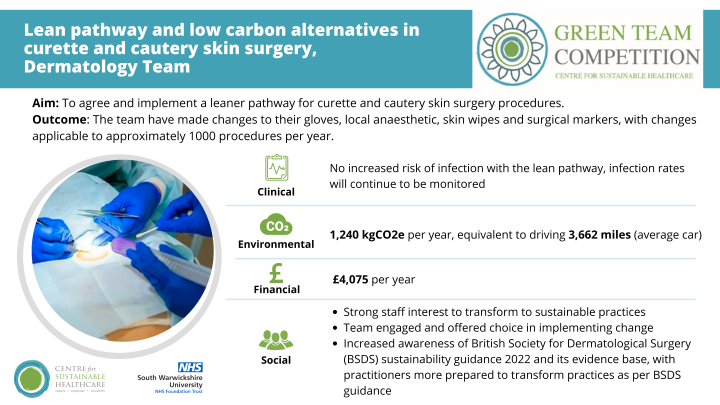
2. Lean pathway and low carbon alternatives in curette and cautery skin surgery, Dermatology team
Summary: Lack of national guidance specifying how skin surgery should be conducted has led to wide variations in practice across the UK. The British Society for Dermatological Surgery (BSDS) sustainability guidance 2022 provided the first UK wide recommendations on environmentally sustainable skin surgery that compliments existing guidance for safety. Curette and cautery minor skin surgery procedure is one of the most performed procedures at the Dermatology Department at SWFT (estimated up to 1,000 procedures per year) and as identified by the project team as having the most potential scope for transformation to more sustainable practice.
Team members: Simon Tso, Consultant - Dermatologist; Tracey Williamson - Staff Nurse; Mi Joo Choi - IMT1; Becky Seeley - GP ST3; Enenche Edache - GP ST3
Aim: Develop consensus on a lean pathway (including adoption of low carbon alternatives) for curette and cautery skin surgery procedures and evaluate the clinical, social, environmental and financial outcomes of this lean pathway.
Method & Impact
The team engaged staff (clinicians, nursing and support staff) within and outside SWFT to explore views and perceived barriers on transformation to sustainable skin surgery practices. The team informed the dermatology department on the evidence and recommendations stated in the BSDS guidance at a departmental meeting.
The team observed strong staff interests to transform to sustainable skin surgery practices however a lack of awareness of the BSDS sustainability guidance 2022 and its evidence base. Curette and cautery procedures were targeted as they were perceived as of lower infection risks and practitioners would be more prepared to transform to sustainable skin surgery practices as per BSDS sustainable guidance.
Process mapping was conducted to describe the existing common practices amongst departmental staff when performing curette and cautery skin surgery and a new lean pathway was proposed for staff to consider adopting as their standard practice. The lean pathway switched from sterile gloves to clean nitrile gloves, switched from using 2.2ml glass vial to 20ml glass vial of local anaesthetic, removed the need for an alcohol skin wipe and reused surgical markers.
With adoption of the new lean pathway, the team anticipate annual savings of £4,075 and 1,240 kgCO2e per year, equivalent to driving 3,662 miles in an average car. Clinically, there has been no increased infection rate. The project team plan to disseminate findings and learning to influence other dermatology departments across the UK, as well as other specialities that perform the same type of procedure, to adopt new sustainable practices.
3. Reducing Continence products waste, Neuro rehab team
Summary: Continence is important for maintaining health, dignity and wellbeing. For many patients in the neurorehabilitation setting, they will have varied levels of incontinence and require continence products and support. While individual continence products are relatively low in cost, as a team we observed many products to be wasted and disposed of without patient use, contributing unnecessarily to our Trust carbon footprint.
Leamington Spa Hospital houses the Central England Rehabilitation Unit (CERU), which offers neuro rehabilitation to adults following acquired brain injury. 3 of 4 wards from the Neurorehabilitation service contributed to this project, 2 Acquired Brain injury rehabilitation wards (42 beds) and 1 stroke rehabilitation ward (20 beds).
Team members: Kathy Wagstaff - Clinical Lead Nurse; Abbie Cooke and Gill Turberfield - Ward Coordinators; Babitta Rani, Sandra Timms - Ward Clerks; Avril Baker, Nicola Compton and Fiona Franklin - Housekeepers
Aims: To understand how many vernicare continence items were being disposed of unused, and to reduce this wastage via education to the clinical team.
Method & Impact
The team completed 4 weeks of observations within the participating wards to identify how many Vernicare products were being disposed of un-used and therefore wasted. The 6 items targeted included male and female urinals, bed pan holders and liners, and vomit and wash bowls. The team observed an average of 25.5 items wasted per day prior to their intervention.
After the 4 weeks, the team presented their findings to the clinical team encouraging staff to be mindful of this waste and to check what patients already had at their bedside before taking more equipment to a patient.
Following intervention, the team observed an 80% reduction in wasted products, saving 20.5 items per day. Projected across a year, this will save 588 kgCO2e, equivalent to driving 1,725 miles in an average car. The reduction will also save £2,222, the majority from reduced procurement of items (2% of this saving is from a reduction in macerator electricity and water consumption).
Socially, the team have engaged the wider neuro rehab team, increasing awareness of how wastage not only impacts on the clinical budget but also the environment. The team plan to continue observations weekly to keep an up-to-date record of the number of items that have been wasted and to continue to remind staff to be mindful of how they manage stock at nursing handover meetings 3 times a day. This will support us to ensure that our change is embedding into everyday practice for the team. They are also considering additional items they could target for further waste reduction.

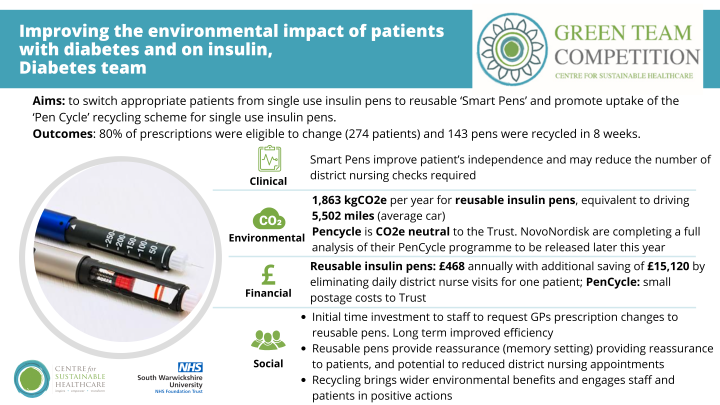
4. Improving the environmental impact of patients with diabetes and on insulin, Diabetes team
Summary: In 2021, the number of people living with diabetes in the UK hit an all-time high at over 4.9 million, with an additional 13.6 million people at increased risk of type 2 diabetes. Individuals with diabetes taking insulin will use a pen device with an insulin cartridge inside. The majority of insulin pens are single use (with 300 units of insulin per pen), and it isn’t possible to know when or how much insulin was last given. Once the 300 units are finished, the needle is removed and the pen disposed of in general waste, therefore creating significant plastic and medication waste. Patients with diabetes are particularly vulnerable to effects of climate change such as extreme weather events and air pollution, due to factors such as impaired responses to heat stress, diabetes-related comorbidities, insulin resistance and chronic low-grade inflammation.
‘Smart Pens’ are reusable pens developed by Novo Nordisk. The pens last 5 years and require much smaller (still single use) cartridges compared to single use pens. Smart pens also provide the time and dose of insulin given on the pen. Novo Nordisk has also set up and advertised a recycling system for single use insulin pens called PenCycle, aiming to reduce the impact when single use pens are still required.
Team members: Angela Cross - Diabetes Dietitian; Hayley Allsopp - Diabetes Specialist Nurse; Georgia Homer - Diabetes Dietitian; Nicky Suddick - Diabetes Specialist Nurse; Claire Bird - Diabetes Specialist Nurse
Aims:
To reduce the environmental impact of insulin pens by:
- switching appropriate patients from single use pens to reusable ‘Smart Pens’
- raising awareness of and promoting use of the ‘Pen Cycle’ recycling scheme for single use insulin pens
Method & Impact
The team reviewed clinic caseloads to identify patient suitable for switching to a reusable Smart Pen or recycling their single use pens. They have started to transfer suitable patients over following education to the patient and engagement with the patients GP to change ongoing prescriptions. The team have encouraged patients with single use pens to recycle, providing Novo Nordisk ‘pencycle’ recycling boxes (which fit 12 pens per box) for patients to fill and return.
Many diabetic patients are seen by the District Nursing teams. At insulin safety week 15th - 19th May 2023 the team promoted recycling to the four community district nursing teams within north Warwickshire. They subsequently ran a competition between the district nursing teams, to collect as many disposable insulin pens as possible in a set timeframe, with a prize offered to the team who recycled the most. Training with district nursing teams in how to use the Smart Pens to implement switching to reusable pens with their caseloads as well has been arranged.
If 80% of suitable patients moved to reusable prescriptions in the next year (274 patients), 1,863 kgCO2e would be saved per year, equivalent to driving 5,502 miles in an average car. There would be a cost saving of £468. This excludes costs of smart pens currently provided for free.
Socially for staff, there may be an initial time investment required to write to GPs and request prescription changes. However long-term improved efficiency and the potential to reduce appointments would lead to larger time savings.
Socially for patients and carers, reusable pens may provide reassurance as pens have memory of the most recent dosage and time given. This could also improve independence, as some patients may be able to give their own insulin at times carers/district nurses were previously required to perform checks. This has been the case for one patient who previously required two checks per day as he had difficulty remembering if he had administered his insulin. The first visit has now been eliminated, as the District Nurse can check the pens memory to confirm that the first does was given correctly. Decisions to reduce visits need to be made jointly with patients and according to clinical judgement of risks, however could bring significant additional financial and caron savings to the Trust. At approximately £45 per District Nurse visit for insulin administration this is a potential saving of £1,260 per month, or £15,120 per year for one patient alone (assuming 28 appointments a month).
PenCycle was cost and carbon neutral for the Trust. While this won’t support the Trust in lowering CO2e emissions, the overall recycling programme is still of beneficial to the environment, by extending the life of material and reducing the need for virgin materials. There are also additional benefits of staff and patients feeling motivated to be taking sustainable actions.
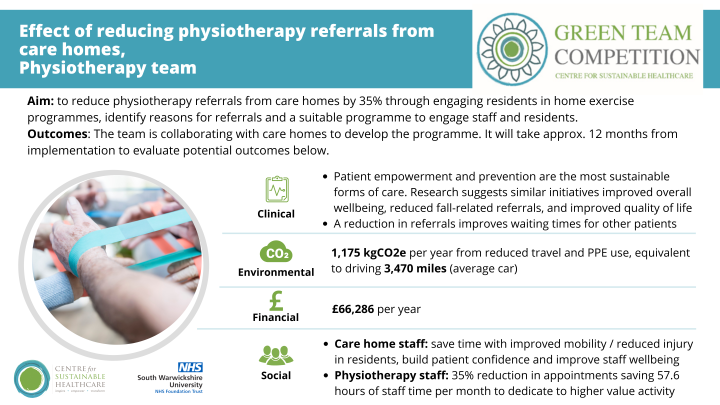
5. Effect of reducing physiotherapy referrals from care homes on waiting lists through health promotion, physical activity, and falls prevention, Physiotherapy team
Summary: Physiotherapists promote health and well-being to restore movement, mobility, function, and self-confidence through exercise, education, and other evidence-based treatments. Long waiting lists for appointments within the NHS have been an ongoing issue for some time with the NHS long term plan aiming to shift models of care further upstream with a focus on preventive care, closer integration of services within the community for people with chronic conditions and reduce outpatient visits by a third. There are strong links between improved public health and reduced need to access healthcare and the NHS carbon footprint. This presents an opportunity to our physiotherapy service, to promote improved care and outcomes for patients, while minimising the environmental, social and financial costs of our care.
Team members: Alison Harbon – Professional Lead; Rachael King – Professional Lead; Sophie Knight – Band 7 Clinical Specialist Physiotherapist; Oluwadamilola Asaju – Band 6 Physiotherapist, Urgent Therapy; Lakshmi Krishnaswamy – Band 6 Occupational Therapist, Urgent Therapy; Aathira Shaji – Band 5 Physiotherapist, Routine Therapy; Rebecca Draper – Band 4 Therapy Assistant, Falls Pathway
Aim:
- Long-term: to reduce physiotherapy referrals from care homes by 35% through engaging care home residents in home exercise programmes. They anticipated several benefits, including improved quality of life for residents, reduced waiting times for referrals, reduced carbon emissions associated with appointment travel, and saving money and staff time
-
Short-term: to identify reasons for referrals; to identify a suitable programme for care homes; to engage care home staff and residents while keeping in mind the long-term measurements; and to estimate benefits across the triple bottom line (social, environmental, and financial).
Method & Impact
The team completed an analysis of their routine caseload, a comprehensive literature review, and engaged key stakeholders top commence the process of developing a home exercise programme (HEP) that will target strength and balance training to improve static and dynamic sitting and standing balance to minimize the risks of falls. The programme is undergoing development and will be trailed in two care homes, with the aim to role out to all care homes, with a focus on empowering care home staff and patients. The programme will be implemented remotely via virtual meetings as much as possible. When face to face meetings are required, we would aim to link these to a patient visit to maximise our savings as detailed below.
It will take approximately a year to measure clinical outcomes for care home residents, however based on the evidence base, benefits of similar initiatives include improved overall wellbeing, reduced fall-related referrals, and improved quality of life. A reduction in referrals may improve waiting times for other patients which may prevent further deterioration in their condition.
With the programme implemented across all care homes and a 35% reduction in referrals achieved, they anticipate a saving of 1,175 kgCO2e per year from reduced travel and PPE, equivalent to driving 3,470 miles in an average car.
With a 35% reduction in appointments (38.36 appointments per month) and a cost of £144 per one-to-one appointment, this equates to a saving of approximately £5,524 per month, or £66,286 per year. There would be an additional saving from the cost of fuel which has not been calculated.
The physiotherapy team would save 57.6 hours, or 7.7 days of staff time per month to dedicate to higher value activity. This may exclude time taken for receiving and triaging referrals, scheduling appointments, and any time dedicated to writing patient notes and programmes.
With a health improvement for patients, care home staff may save time as residents require less support and referrals. Seeing patients engage more in exercise and build confidence may improve staff wellbeing. With care home staff implementing HEP’s there are potential positive or negative impacts – staff may enjoy learning, empowerment and taking on a new role/responsibility, or may feel this is a task added to add to already demanding workloads.
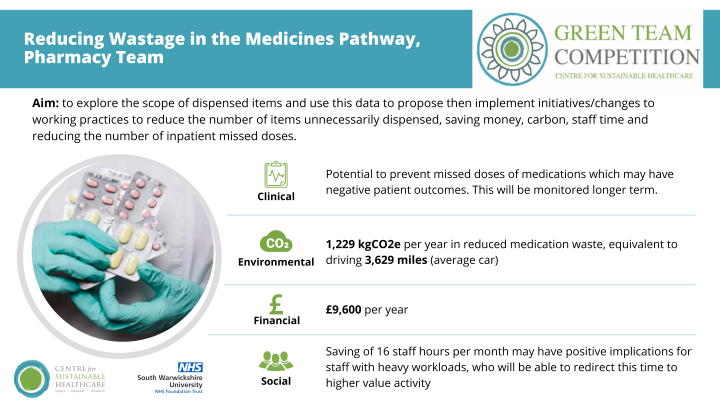
6. Reducing Wastage in the Medicines Pathway, Pharmacy team
Summary: For some time the pharmacy team have been aware of unnecessary or duplicate dispensing happening in the Trust. A previous project targeting return of dispensed medications that would go un-used (and be discarded) has achieved financial savings of £61,682 and 7,895 kgCO2e.
However, the team have questioned why so much duplicate dispensing is happening in the first place. Professional experience has shown that some proportion of medicine supplies are in fact unnecessarily re-dispensed items. This can happen for a variety of reasons (damaged medicines, increased dosage/frequency) but one of the more impactful from the perspective of patient care is to do with transfer. When patients move bed space or ward, it is not always the case that medicines are transferred with them. This not only leads to items being requested again, but it also leaves the patient in the new location without the medicines that we have dispensed for them, which in turn may lead to missed doses. Depending on the medicines in question, this could have a significant detrimental impact on the patient (e.g. when doses of medicines for the treatment of Parkinson’s disease are missed).
Dispensing medicines unnecessarily also results in increased stockholding, which is known to increase waste through expired/damaged medicines We therefore concluded that there would be value in exploring our suspicions further, with the aim of reducing the volume of medicines entering the pathway (and therefore the waste stream) and ensuring that medicines are available for patients when they need them.
Team Members: Tessa Dadley - Lead Technician, Procurement & Goods-Receipt; Colin Foy - Pharmacy Operations Manager; Louise Foy-Coley - Lead Technician, Dispensary, Distribution & Training; Sarah Welsby - Lead Technician, Ward-Based Medicines Management
Aims:
- short term (during competition period): to explore the scope of dispensed items and use this data to propose initiatives/changes to working practices to reduce the number of items unnecessarily dispensed
- long term: to implement proposed initiatives/changes to working practices to reduce the number of items unnecessarily dispensed, saving money, carbon, staff time and reducing the number of inpatient missed doses
Method & Impact
The team collected data over a one month period. Data gathering was driven by dispensers to identify requests for unnecessary resupply which can be seen on pharmacy systems. This enabled us to understand the extent of the problem and reasons for redispensing, and to inform plans for change ideas.
In the month there were 243 re-dispensed items accounting for 4% dispensing undertaken. Projected across a year this equates to 12,288 kgCO2e with a total drug-cost value of £96,000. This represents approximately 12 hours of dispensing time and 4 hours of accuracy checking time per month, at a staffing cost of approximately £2.5k per year.
As a conservative estimate, if they reduced their re-dispensing by 10% in the next year, they would save £9,600 and 1,228.8 kgCO2e per year, equivalent to driving 3,629 miles in an average car.
Socially, an estimated saving of 16 staff hours per month may have positive implications for staff with heavy workloads who will be able to redirect this time to higher value activity. Clinically, it is possible to monitor missed-dose data (which is already available/collected), to observe if a reduction in re-dispensing can support a reduction in missed medication doses. This may have wider implications on length of stay, which in turn increases the CO2e and financial costs of a patients admission.
The team plan to present their findings to the wider team, and while specific actions require more investigation, initial suggestions include:
- a communications campaign to share these findings with ward staff, to increase awareness and promote medicines transfer
- a change to patient transfer procedures to include ‘empty bed, open lockers’ initiative, which would ensure transfer of all locker contents including medicines
- addition of a check for porters when handing over medicines in admissions areas, to ascertain if the patient has moved in the time taken to dispense the requested medicines and facilitate transfer
Awards
 Congratulations to the winning team, the Care of the Elderly Team for their project to reduce low value blood testing in care of the elderly and frailty wards. The project team were praised by the judges for their long-term thinking to ensure longevity of staff behaviour change and the projects beneficial impacts across the full sustainable value equation.
Congratulations to the winning team, the Care of the Elderly Team for their project to reduce low value blood testing in care of the elderly and frailty wards. The project team were praised by the judges for their long-term thinking to ensure longevity of staff behaviour change and the projects beneficial impacts across the full sustainable value equation.
The Centre for Sustainable Healthcare would like to thank and congratulate all teams that took part in the competition. The competition's outcomes serve as proof of the teams' commitment and efforts to improving the sustainability of the healthcare system.
“It is fantastic that clinicians from across the organisation are committed to embedding environmental and sustainable practices into their areas of work. As a large organisation, we recognise the role we and the wider NHS, need to play in tackling the climate crisis and clinical and operational involvement is key to this. All the projects we have seen are brilliant examples of how big or small changes can make an impact. The enthusiasm shown by the teams is great, and I can’t wait to work with more teams across the organisation.” - Dr Charles Ashton, Chief Medical Officer
Acknowledgments
Thank you to Cristina Calleja, Senior Sustainability Manager and Caroline Lloyd, Sustainability Officer at SWFT for partnering with us in the competition and supporting the teams.
Thank you to our judging panel.
Thank you to our SWFT SusQI Academy members who supported the Green Teams alongside their SusQI Academy work:
- Lorna Bannan, OPMU project officer
- Cristina Calleja, Sustainability Manager
- Faye Kenning, Service improvement Manager
- Emma Rowan, Service improvement Manager
- Joanne DulsonCox, Quality Assurance Manager

