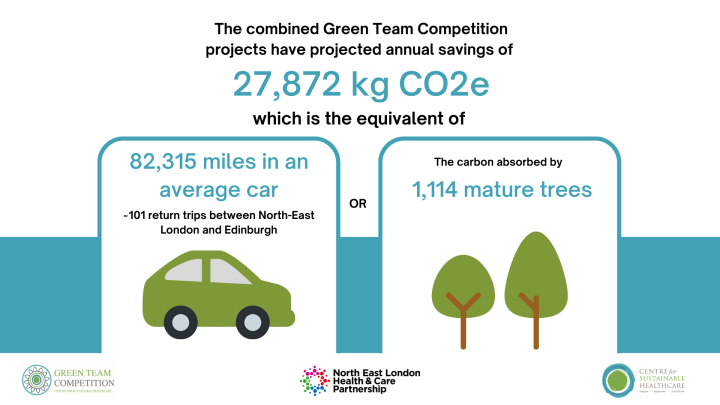
North East London Health and Care Partnership Green Team Competition expected to save £231,518 and 27,872 kgCO2e annually
As part of their journey towards a net zero health and care system, North East London Health and Care Partnership commenced a Green Team Competition in partnership with the Centre for Sustainable Healthcare in May of this year.
The competition has brought anticipated annual savings of £231,518 and 27,872 kgCO2e. This is the carbon footprint equivalent of driving 82,315 miles driven in an average car or 101 return trips between North-East London and Edinburgh.
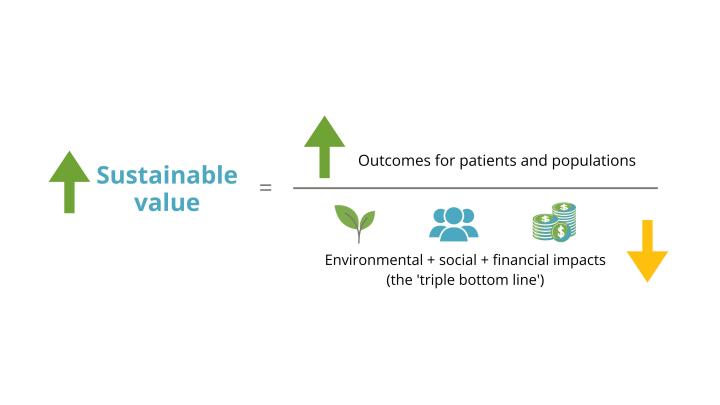
Through the Green Team Competition, 5 teams were selected from across 4 organisations within the partnership from both primary and secondary care to engage in our sustainability in quality improvement (SusQI) programme to transform knowledge into action. Each team received mentoring from CSH facilitators to drive healthcare transformation by developing, implementing and measuring the impact of projects through the lens of the sustainable value equation.
 Teams presented their projects to a virtual judging panel on the 24th October. The judging panel included:
Teams presented their projects to a virtual judging panel on the 24th October. The judging panel included:
- Jo Moss, Chief strategy and transformation officer, NHS North East London
- Steve Collins, Director of Finance, NHS North East London
- Annie Palstam, CSH Associate, Professor, physiotherapist, and senior lecturer at the Institute of neuroscience and physiology and Chair of the Council for ethics and sustainable development, Swedish Association of Physiotherapists.
The projects were then showcased via poster presentations at an in-person NHS NEL Net Zero celebration event. The Winning and Highly Commended teams were announced here, and both were invited to present their project to an appreciative audience on the day.
Thank you to Rebecca Waters, Health Improvement and Inclusion Manager – Net Zero and Anchor Organisations, NHS North East London, Part of North East London Health and Care Partnership for collaborating with us in the competition and hosting a wonderful celebration event.
Green Team Competition Projects
Read the full Impact Report here or view the project summaries below.
- Dentistry Team, Barts Health NHS Trust
A) Incorporating the use of haptic simulators in dental education and engaging students in sustainable practice
B) Remote Consultations in Dentistry - Estates Team, East London NHS Foundation Trust, Reusable safe cutleries and plates at John Howard Centre
- Food Strategy Team, Partnership with Tolworth Medical Centre and Newham Council, Food Growing in Health and Care settings in Newham
- Woodberry Wetlands Primary Care Network (PCN): The Heron Practice and Allerton Road Medical Centre, Reducing the environmental impact of inhalers in patients with asthma across a PCN
- Physiotherapy Team, Royal London Hospital, Barts Health NHS Trust, The environmental impact of specialist physiotherapy for limb reconstruction: a SusQI project
1. Dentistry Team
The Dentistry team completed two projects.
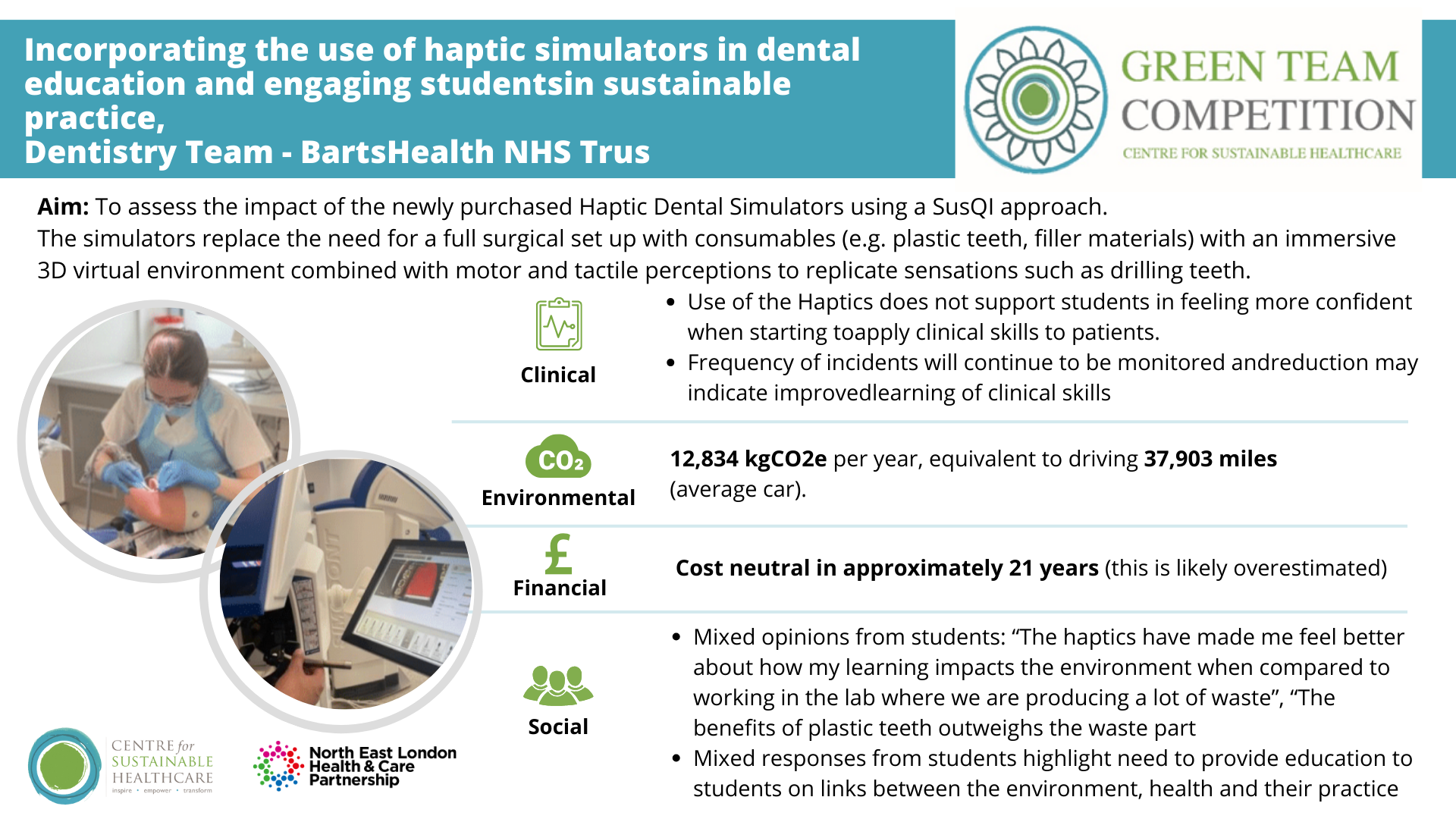
Project 1: Incorporating the use of haptic simulators in dental education and engaging students in sustainable practice
Summary: The acquisition of manual dexterity and tactile sensory surgical skills are essential in Dentistry. Conventionally, students learn pre-clinical skills through practicing to drill plastic teeth on phantom (dummy) heads. This method is non-patient facing, however replicates the full surgery set up utilising PPE, drills, single use cutting burs, filling materials, instruments and single use consumables (e.g. suction, barrier coverings, filling materials).
Queen Mary Institute of Dentistry has invested £1.7 million on 42 Simodont Haptic simulators (at a cost of £41,000 each). Haptic simulators utilise an immersive 3D virtual environment combined with motor and tactile perceptions to replicate sensations such as drilling teeth. Students can start to practice these skills earlier (in year one of study) with feedback given continuously and instantaneously via the simulator.
Team members: Project lead - Zahra Shehabi (Consultant in Special Care Dentistry; Alessandra Booth (Dental Core Trainee and Academic Clinical Fellow); Giulia Pintaritsch (4th Year Dental Student)
Aim: To assess the impact of the newly purchased Haptic Dental Simulators across the triple bottom line (social, environmental and financial) using a SusQI approach.
Method & Impact: The simulators were purchased and first used in October 2022 and have been used intermittently since. A full roll out from September 2023 is planned. Process mapping was undertaken to identify areas where savings in social, environmental and financial resource use could be achieved using the Haptic simulators.
Data items saved on the haptics server showed that undergraduates in Year one and Year three are the main users of the haptic simulators. To ensure a like-for-like comparison between the conventional method using plastic teeth and the haptic simulator, BDS year one items saved were removed from the data totals of the Haptic simulator as students do not start practicing pre-clinical skills using the conventional method until their second year. This resulted in a total of 1040 items saved over a six-month period.
Projected across a year, use of the Haptics simulator saves 12,834 kgCO2e, equivalent to driving 37,903 miles in an average car. The team estimated 21 years for the Haptics Simulators to be cost neutral based on assumptions and lowest costs for the traditional method however this is likely an overestimation as they needed to reply on simulator data saved by students to assume usage, and there is potential for a wider range of students to use the device.
Socially, and with potential impacts clinically, students had mixed opinions on use of the Haptics Simulators, with only a third reporting they prefer the haptic simulator method.
“The haptics have made me feel better about how my learning impacts the environment when compared to working in the lab where we are producing a lot of waste” - Student A
“The benefits of plastic teeth outweighs the waste part” - Student B
As a result, an engagement initiative with students was launched including clinician input into the student prevention volunteering programme, Barts Community Smiles, to incorporate sustainability into the preventative advice given to members of the community and a workshop arranged with students on sustainability in dentistry.
Project 2: Remote Consultations in Dentistry
Summary: Video and telephone consultations were introduced at the Royal London Dental Hospital during the COVID-19 pandemic when access to dental services had completely ceased nationally. Even in the ensuing months where dental practice had resumed, access remained limited, especially for vulnerable populations who were at a greater risk of contracting the virus, who form the majority of our patient cohort in secondary care. To date, there has not been a service evaluation ascertaining the extent of use, frequency, economic, social or environmental impacts.
Part of the focus was on Special Care Dentistry (SCD), a specialty that provides dental care for adult patients with additional medical, social, psychological, physical, or sensory needs (e.g., dementia, bed bound patients, learning disabilities). Being a secondary care specialist referral centre, the clinicians in the service currently treat only the most complex patients within these groups, and for many patients access to dental services is challenging.
Team members: Zahra Shehabi, Consultant in Special Care Dentistry, z.shehabi@nhs.net; Alessandra Booth, DCT2 in Dental Public Health, alessandra.booth@nhs.net
Aim: To evaluate the sustainable value use of remote consultations (via video or phone) at Barts Dental Hospital over a two-year period.
Method & Impact: 165.5 special care patient consultations and 1,674 ‘other specialty’ consultations took place across one year. This is a saving of 10,807 kgCO2e, equivalent to driving 31,916 miles driven in an average car, from a reduction in patient travel and consumables used for a standard dental examination. Based on reduced consultant time and average costs of an outpatient face to face consultant, £163,943 will be saved annually, and an estimated £9,271 will be saved from consumable use per year.
Clinically, most staff agreed remote consultations have improved access to dental care and contributed to positive patient outcomes and facilitated care more efficiently. Over two thirds felt they were able to pick up dental problems more promptly using remote consultations.
Socially, the change increases accessibility to dental care. 94% patients preferred remote consultations over face-to-face consultations for their initial assessment. Each year remote clinics at Royal London Dental Hospital save the equivalent of the working of a 0.5 WTE (whole time equivalent) of a dental nurse. This time can be redirected to higher value work.
Future work is therefore planned to roll our remote consultations across all specialities in the Dental Hospital using the Special Care Dentistry department as a case study to highlight the positive impact this can have in relation to patient feedback, staff wellbeing and sustainability. - Dentistry Team
2. Estates Team, East London NHS Foundation Trust, Reusable safe cutleries and plates at John Howard Centre
Summary: It is estimated that England uses 2.7 billion items of single-use cutlery — most of which are plastic — and 721 million single-use plates per year. A range of polluting single-use plastics (including plastic cutlery, plates and polystyrene trays) will be banned from October 2023 following the Government's consultation.
East London NHS Foundation Trust provides mental health services, including care to patients in forensics wards. A forensic mental health ward provides intensive support for adults and young people with mental health needs in a secure setting. To maintain patient and staff safety during mealtimes, it is not possible to switch to standard metal cutlery. As a team they therefore needed to work together to move towards sustainable mealtimes - lowering our carbon footprint while improving patient dining experiences, maintaining patient and staff safety and reducing procurement costs.
Team members: Jeffrey Sham, Sustainability & Net Zero Officer; Adam Toll, Assistant Director of Estates; Henna Beegun, Clinical Nurse Manager
Aim: To safely replace single use cutlery and plates with reusable alternatives in forensics wards.
Method & Impact: John Howard forensic centre in Hackney has 11 wards. The team identified Clerkenwell Ward, a learning disability unit, as suitable to trial our changes and engaged with the clinical staff in the unit to review and test suitable items of cutlery and plates to ensure patient safety. The team confirmed the equipment they would like to swap to are non-breakable, non-ligature and no risk to service users. Cups were excluded from the current project as some were already reusable and others recyclable.
The Estate team considered how service users (patients) may engage in the change and with clinical staff considered which patients may like to be involved. Patients will be encouraged to take active roles in mealtimes, such as bringing reusables to the dishwashing area. An incentive of a small payment will be offered to patients who take part in this task.
They reviewed all logistical considerations. The unit already had a dishwasher in place and the reuse and sterilisation process was confirmed with suppliers and infection prevention control. All equipment is required to go through an approval process. At present, plates have been approved and silicone cutlery approval is pending. Close monitoring of product inventory and designated patient washing and storing of reusables will be required on an ongoing basis which requires ongoing collaboration between the estates and clinical team.
The team estimate that in the Learning Disability Unit alone, 976 kgCO2e will be saved per year by switching from disposable to reusable cutlery. This is equivalent to driving 2,883 miles in an average car. And save between £3,042 - £3,702 depending on whether 2 or 3 cutlery sets are required (to account for misplaced items).
With success of the trial, there would be opportunity to scale for further savings, where the John Howard Centre alone spends approximately £60,000 per year on single use cutlery (excluding waste disposal costs).
3. Food Strategy Team, Partnership with Tolworth Medical Centre and Newham Council, Food Growing in Health and Care settings in Newham
Summary: The national project Growing Health by Sustain and Garden Organic produced a literature review on: ‘The benefits of gardening and food growing for health and wellbeing’. It found gardening can increase physical activity and fitness, contribute to healthy weight management, increase fruit and vegetable consumption as well as improve mental health via social interaction, community cohesion, reduced stress, and reduced reliance on medication. There are further additional benefits for specific health conditions, such as reducing risks of falls, alleviating agitation in dementia, improvements in pain recovering from surgery and coping with intensive cancer treatments.
Unfortunately, in very urban communities green space is limited and particularly private gardening spaces and this is especially true in less affluent communities. A report in 2019 by Capital Growth and supported by the Mayor’s office explored the barriers to community gardens access via social prescribing. Some of these barriers included limited referrals, low visibility, and a lack of clarity/confidence about what sort of support gardeners would need. However, access to gardens and food growing space is what the community wants. A recent survey on the state of local authority allotment services finds almost 87% of the local councils surveyed have experienced a noticeable increase in demand for allotment plots. As of June 2023, there were a total of 111,566 people on a waiting list for one of the 120,000 council plots across the country.
As part of the Green Team Competition, the team has established a group of professionals representing various stakeholders within the NHS (GP, PCN, GP Federation and ICB level) and Newham Council. A key strength to this approach was allowing us insight into and ability to work across the local healthcare system. Mapping how many gardens we have in NEL Healthcare spaces and how many grey spaces that have potential to be Green is an action in the ICS Green Plan.
Team members: Catherine Gaynor, Newham GP and a Net Zero Clinical Lead for NHS North East London; Patrick Vickers, Regenerative Food Specialist at Newham Council; Nohora Castro Tamara, Social Prescriber, Newham North West 2 Primary Care Network; Julia Briscoe, Clinical Fellow for Personalised Care for NHS North East London; Cliff Mcmahon-Docherty, Personalisation Lead, Social Prescriber, Newham Health Collaborative; Augusta Adu, Newham Senior GP Social Prescriber; Katy Szita, Head of Wellbeing Team, Newham North West 2 Primary Care Network
Aim: To develop a food growing project toolkit incorporate SusQ recommendations to be made available to all health professionals working in Newham with an interest in developing a food growing/gardening club for their patients and staff.
Method & Impact:
- The team engaged key stakeholders (PCN, Federation, Council, ICB) and conducted an evidence review to inform the toolkit on the benefits of food growing and green social prescribing. The intention of this was to prove the concept and impact to policymakers and the health care system.
- The practicalities of a garden set up and patient recruitment were collected from the experiences of the gardening stakeholder members.
- Funding options and ideas discussed and included in the toolkit.
The team liaised with wider teams and network of GP practices to identify food growing and gardening projects currently underway that maybe suitable to highlight as case studies. A local project was identified that demonstrated positive health and social impacts as reported by patients. Unfortunately, it was not possible to obtain data for measuring more specific clinical, financial, or environmental (including CO2e) impacts. (Partly due to clinical time constraints plus limited recorded data collection in relation to gardening projects identified).
Next steps: The team have considered options for how and which measurements may be embedded into future gardening projects, such as by updating ICB templates for social prescribing, embedding into systems such as EMIS and using the JOY social prescribing platform. The answer to this still needs further development at a NEL IT level.
They aim to promote the toolkit to all health professionals working in Newham with an interest in developing a food growing/gardening club for their patients and staff. Sharing this resource plus information/evaluation of first project(s) delivered more widely in North East London and nationally to showcase this as a green social prescribing initiative taking place in Newham. The team would also like to feed back to policy circles to justify further investment into new food growing spaces.
This project has brought people together from across the whole system. Although we haven't yet been able to make specific carbon savings, it is a great kick start to green space investment for healthcare settings, residents and staff in Newham and NEL. Investment that will lead to environmental benefits (including carbon reduction) in lots of hard to measure ways! - Estate Team
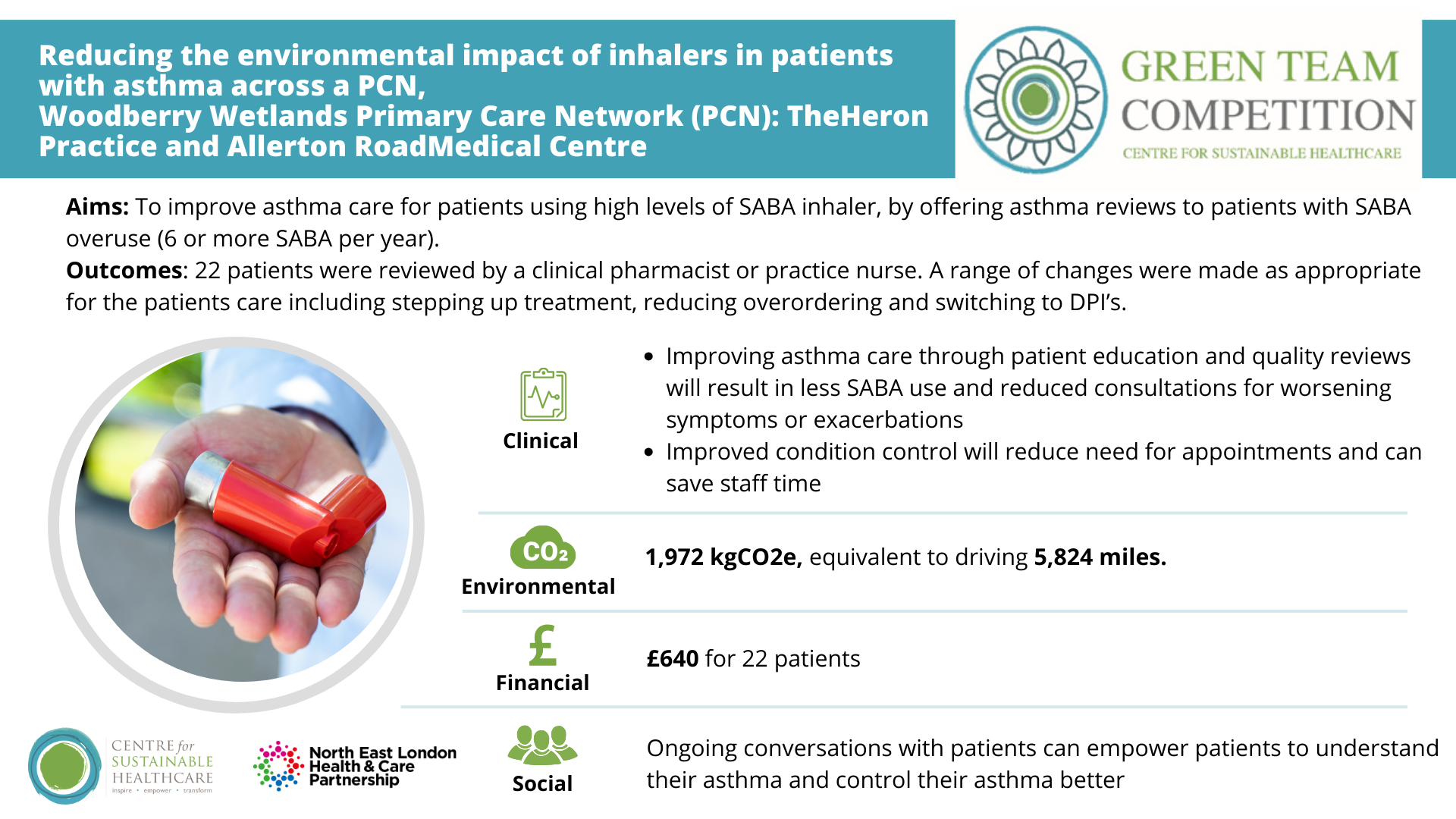
4. Woodberry Wetlands Primary Care Network (PCN): The Heron Practice and Allerton Road Medical Centre, Reducing the environmental impact of inhalers in patients with asthma across a PCN
Summary: Hydrofluorocarbon/hydrofluoroalkane propellants from MDIs contribute 3.5% of the total carbon footprint of the NHS. Dry powder inhalers (DPIs) have a carbon footprint 18 times lower than MDIs and clinically, DPIs have been proven to be as effective as MDIs. The NEL asthma guidelines have been adapted to reflect the importance of reducing the use of SABA (short acting beta agonists), switching to dry powder inhalers if a patient has appropriate inhaler technique, and focusing on maintenance and reliever therapy in those patients who are overusing SABA.
There are many reasons why patients might over-request SABA, including misunderstanding their asthma management plan, poor inhaler technique, not realising they still have medicine in their inhaler, and having poor asthma control due to lifestyle and environmental factors. Some patients with asthma may have anxiety which can result in overuse of inhalers.
The “Why Asthma Still Kills” National Review report recommends that all asthma patients who have been prescribed more than 12 SABA’s in the last 12 months be invited for an urgent review of their asthma control.
Team members: Mareeni Raymond, GP at The Heron Practice; Humairaa Said, PCN Pharmacist at The Heron Practice; Ruth Hallgarten, GP at the Allerton Road Medical Centre; Joe Larkai, PCN Pharmacist at the Allerton Road Medical Centre; Bharat Uppala, Woodberry Wetlands PCN Pharmacist; Anil Ramyead, Woodberry Wetlands PCN Pharmacist Lead
Aim: To work together as a PCN to improve asthma care for patients using high levels of SABA inhaler to:
- Improve understanding of new asthma guidelines in staff carrying out asthma reviews
- Introduce a system that will promptly alert clinicians of SABA overuse (6 or more SABA per year)
- Arrange asthma reviews with a view to improving asthma care, reducing overuse of SABA and reducing our PCN carbon footprint.
Method & Impact: The team focused on a cohort of patients who had requested 6 or more SABA inhalers in the past 12 months and invited them via text messages for face-to-face reviews. The pharmacists at each practice were briefed about the asthma guidelines and how to discuss greener inhaler prescribing and asthma care and the intention was to incorporate this into discussions with the patient at their reviews.
In the competition timeframe 22 patients were reviewed by a clinical pharmacist or practice nurse. A range of changes were made as appropriate for the patients care including stepping up treatment, reducing overordering and switching to DPI’s. Based on the 22 patients, the team anticipate annual savings of £640 and 1,972 kgCO2e, equivalent to driving 5,824 miles in an average car. Changes made will improve, or at a minimum maintain, asthma control and treatment for patients.
Training sessions, to update staff knowledge on guideline-adherent asthma care, are planned in September for pharmacists and nurses which will be lead by Dr Raymond for the PCN prescribing and nursing team. Ongoing conversations with patients can empower patients to understand their asthma and control their asthma better, however staff and patients need to be aware of the many factors that might result in overprescribing and medication overuse.
The practices plan to increase their positive impact by widening the search to identify all asthma patients requesting 6 or more SABA in the past 12 months. The aim is to review all the patients and trialling a new prescription system for SABA inhalers.
5. Physiotherapy Team, Royal London Hospital, Barts Health NHS Trust, The environmental impact of specialist physiotherapy for limb reconstruction: a SusQI project
Summary: People with complex bone injuries require limb reconstruction management, which entails the bones being fixed and potentially adjusted through time with an external fixator device, or circular frame. This is a long process affecting people’s function and daily life with surgeries, medication, imaging, specialist equipment, highly trained personnel and close follow up in specialist clinics needed.
Because of the complexity of the condition, rehabilitation can take second place and physiotherapy is often delegated to third parties (e.g., community or private providers). Lack of specialist physiotherapy during this process can lead to poorer functional outcomes for patients, impacting quality of life, while adding additional financial, social and environmental costs to the NHS.
Team members: Catherine Borra (Physiotherapist and Research Associate, Barts Health NHS Trust); Rebecca Wood (Physiotherapist and Research Associate, Barts Health NHS Trust); Daniel Church (Limb Reconstruction Specialist Physiotherapist, Barts Health NHS Trust); Catherine Hilton (Physiotherapist and Research Associate, Barts Health NHS Trust); Jade O’Brien (Clinical Nurse Specialist, Barts Health NHS Trust)
Aim:
- Estimate the effect of introducing specialist physiotherapy on the limb reconstruction service across the sustainable value equation
- Identify strategies to further improve the environmental efficiency of the limb reconstruction service
Method & Impact: The Royal London Hospital limb reconstruction team (LRT) comprised of consultants, doctors and one specialist nurse. Patients were seen on a nearly weekly basis by a specialist limb reconstruction MDT, with ad-hoc specialist nurse appointments for wound care and adjustments and regular imaging. Once healing has occurred, the circular frame would be removed either in clinic or theatre.
Referrals to physiotherapy would be recommended to the patients GP. Processing and waiting times could be months. In 2020, the LRT employed one full time Band 7 specialist physiotherapist to support the specialist nurse clinics and provide early ad-hoc rehabilitation to limb reconstruction patients. In addition to the standard pathway, patients in the physiotherapy pathway are offered weekly physiotherapy and the opportunity to join two specialist gym sessions a week – which are attended by multiple patients and supervised by the physiotherapist. The physiotherapist also developed skills to assist the specialist nurse in circular frame removals in clinic. As a two-person task, this had required the help of a doctor in the standard pathway (several more staff are required for theatre removals).
Data of 67 patients (28 from the standard pathway and 39 from the physiotherapy pathway) was randomly selected and compared. The team found no significant difference in the number of MDT appointments and imaging required by patients, however, there was an increase in suitability for clinic removal instead of theatre removal. Avoiding the need for patients to go to theatre means not subjecting them to higher doses of anaesthetics, reduced consumables required and less staff required. They identified potential to further reduce the carbon footprint of frame removal by considering a switch from Entonox to a more sustainable anaesthetic (e.g. Penthrox).
- 30% increase in clinic frame removal instead of in theatre. Clinic removal frees theatre time for other procedures and allows patients to have their frame removed sooner.
- Over 70% patients reported positive outcomes (returned to baseline function or independently mobile) with physiotherapy, compared to 60% negative outcomes (further intervention, ongoing pain or functional deficits) in standard pathway.
Based on a caseload of 120 persons per year, the team anticipate savings of 1,283 kgCO2e, equivalent to driving 3,789 miles. This is a 20% reduction in frame removal emissions. Further reductions could be achieved with consideration of a shift from Entonox to a more sustainable anaethetic gas (e.g. Penthrox). Accounting for investment in a band 7 physiotherapist, the pathway saves £54,622 a year, a 23% reduction in frame removal costs. And saving significant staff time from the shift from theatre to clinic room removal as additional staff are required in theatre, and two staff are required in clinic. These savings are likely underestimated, as they do not account for reductions in further care that would be required with more complications and poorer functional outcomes in the standard pathway.
The limb reconstruction clinical team are very positive about the physiotherapy pathway and recognise the value in bespoke physiotherapy that considers the differences in each patient’s presentation. However, they highlight the need to improve measurement of patient outcomes as a way of monitoring success and continuing to improve the service.
Awards
 Congratulations to the Physiotherapy team for winning North East London Health and Care Partnership Green Team Competition 2023! The project team were praised by the judges for a project that engaged a multidisciplinary team while highlighting AHP value in early intervention to optimise patient outcomes.
Congratulations to the Physiotherapy team for winning North East London Health and Care Partnership Green Team Competition 2023! The project team were praised by the judges for a project that engaged a multidisciplinary team while highlighting AHP value in early intervention to optimise patient outcomes.
Congratulations to the highly commended team – Food Strategy! Creation of a food growing for patients toolkit has brought people together from across the whole system (PCN, Federation, Council, ICB, GPs) and is a great kickstart to promote green space investment for healthcare settings, residents and staff in Newham and NEL.
The Centre for Sustainable Healthcare would like to thank and congratulate all teams that took part in the competition. The competition's outcomes serve as proof of the teams' commitment and efforts to improving the sustainability of the healthcare system.