
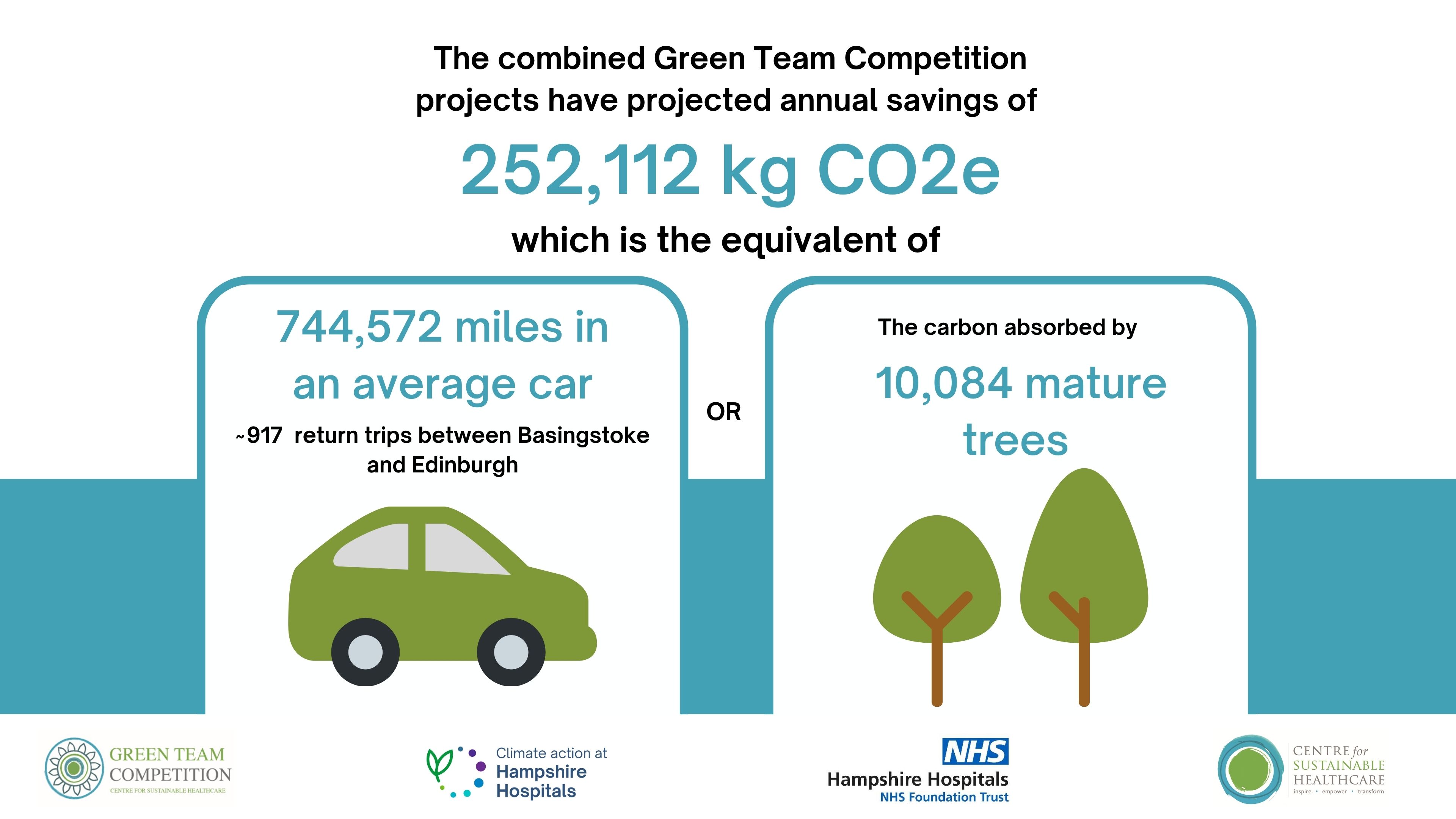
Hampshire Hospitals NHS Foundation Trust Green Team Competition expected to save £ 443,119 and 252,112 kgCO2e annually
In June of this year, Hampshire Hospitals NHS Foundation Trust (HHFT) commenced a Green Team Competition in partnership with the Centre for Sustainable Healthcare. The competition has brought anticipated annual savings to the Trust of £443,119 and 252,112 kgCO2e. This is the carbon footprint equivalent of driving 744,572 miles in an average car (or 917 return trips between Basingstoke and Edinburgh).
Through the Green Team Competition, six teams from HHFT were selected to engage in our award-winning programme in sustainability in quality improvement (SusQI) that transforms expert knowledge into action. Each team received mentoring from CSH facilitators to drive healthcare transformation by developing, implementing and measuring the impact of projects through the lens of the sustainable value equation.
 At the November 28th Showcase and Awards Ceremony, the teams presented their projects, including the anticipated savings and opportunities to scale and spread, to an audience from the Trust and the judging panel including:
At the November 28th Showcase and Awards Ceremony, the teams presented their projects, including the anticipated savings and opportunities to scale and spread, to an audience from the Trust and the judging panel including:
- Alex Whitfield, Chief Executive, HHFT
- Shirlene Oh, Chief Strategy and Population Health Officer, HHFT
- Tamara Everington, AMD for Change, HHFT
- Louise Fox, Associate Director Nursing, HHFT
- Rachael Ward, Networks Lead, The Centre for Sustainable Healthcare
Green Team Competition Projects
Read the full Impact Report here or view the project summaries below.
- Reducing medicine waste, Pharmacy team
- Outpatient parenteral antimicrobial therapy (OPAT) service at Hampshire Hospitals Foundation Trust (HHFT) in the Net Zero NHS, OPAT team
- Reducing CO2 waste through implementing remanufactured harmonic scalpels in laparoscopic surgery and replacing disposable surgical gowns with reusable surgical gowns, Theatres team
- HHFT Glove Use Awareness Campaign, Infection prevention and control team
- Reducing low value activity in the emergency department, Emergency team
- Reducing The Amount of Wasted Food in Hampshire Hospitals Foundation Trust, Catering team
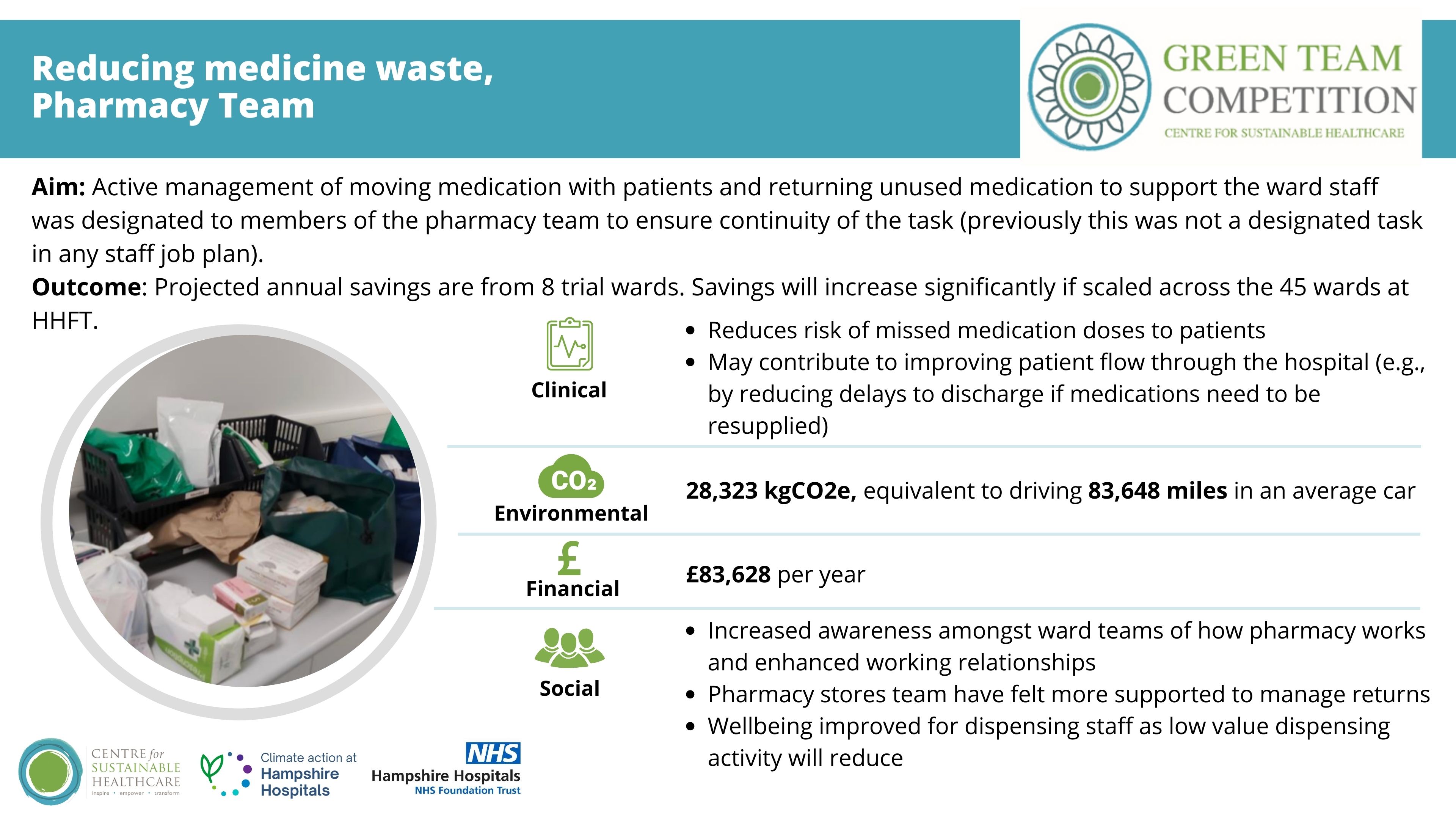
1. Reducing medicine waste, Pharmacy team
Summary: Medicine waste is a huge problem across the NHS. It is estimated that £300 million is wasted annually on unused or partly used medication. Within the hospital setting, medication waste is largely contributed to by patients not taking their medications home, or medications not being transferred with them during their inpatient journey (e.g., if they move wards).
If this medication is not given to the patient they could miss important doses of critical medication resulting in longer length in-patient stays as their health may decline. If medications are missed at discharge, the discharge could be delayed as a new dispensation request is sent, or the patient may remain unwell which may lead to an avoidable readmission.
The reasons behind this project was to look at the dispensing that is carried out by the pharmacy team that does not reach the patient and either has to go through a tedious process of returning the medication back into stock or as is most often the case being disposed of as clinical waste.
Team members: Claire Williams, Deputy Clinical Pharmacy Manager; Louise Bond, Deputy Lead Medicines Management Technician; Stacey White, Medicines Management SATO; Emily Green, Medicines Management SATO; Atlanta McLauchlan, Medicines Management SATO
Aim: to reduce waste by moving patients’ medication with them and returning unused medication in a timely manner so it can be reused (not disposed of).
Method and impact: Before the project there was no clear designation of responsibility across stores, ward teams and dispensaries resulting in a large volume of medication waiting in the returns area.
One staff member on each of the two sites was therefore designated the responsibility of active management of moving medication with patients and returning unused medication to support the ward staff. This staff member would visit allocated wards. at least 2 to 3 times a week and they check the treatment room and TTO cupboards to see if any medication has been left there due to the patient going home or moving to another ward. For medication that is not required they will assess if it has been stored correctly and is still in its original container with at least 3 months expiry left and if it meets this criteria it will be returned into stock to be reused. For patient transfers they will double check which ward they have been moved to and liaise with the Pharmacy team covering the ward to ensure that the medication is still required by the patient. This meant there was continuity to the task. The team identified 8 trial wards (4 per site) to implement a trial of this process.
Across a month trial period, the team observed an increase return in medication to the cost of £6,942, equivalent to 2,360.28 kgCO2e, equivalent to 6,970 miles driven in an average car. Savings from waste disposal (incineration) were approximately £27.00 and 32 kgCO2e in reduced incineration costs.
Socially, the project has increased awareness amongst ward teams of how pharmacy works and enhanced working relationships. The pharmacy stores team have felt more supported to manage returns and wellbeing has improved for dispensing staff as low value dispensing activity will reduce. The project also reduces risk of missed medication doses to patients and may contribute to improving patient flow through the hospital (e.g., by reducing delays to discharge if medications needing to be resupplied).
Due to the project’s success, a new member of staff is being employed on the RHCH site so that there will be two staff members to support more wards on each site. Long term the team are also exploring the impact of not supplying patients’ regular medication on discharge when the inpatient stay was less than 72 hours.
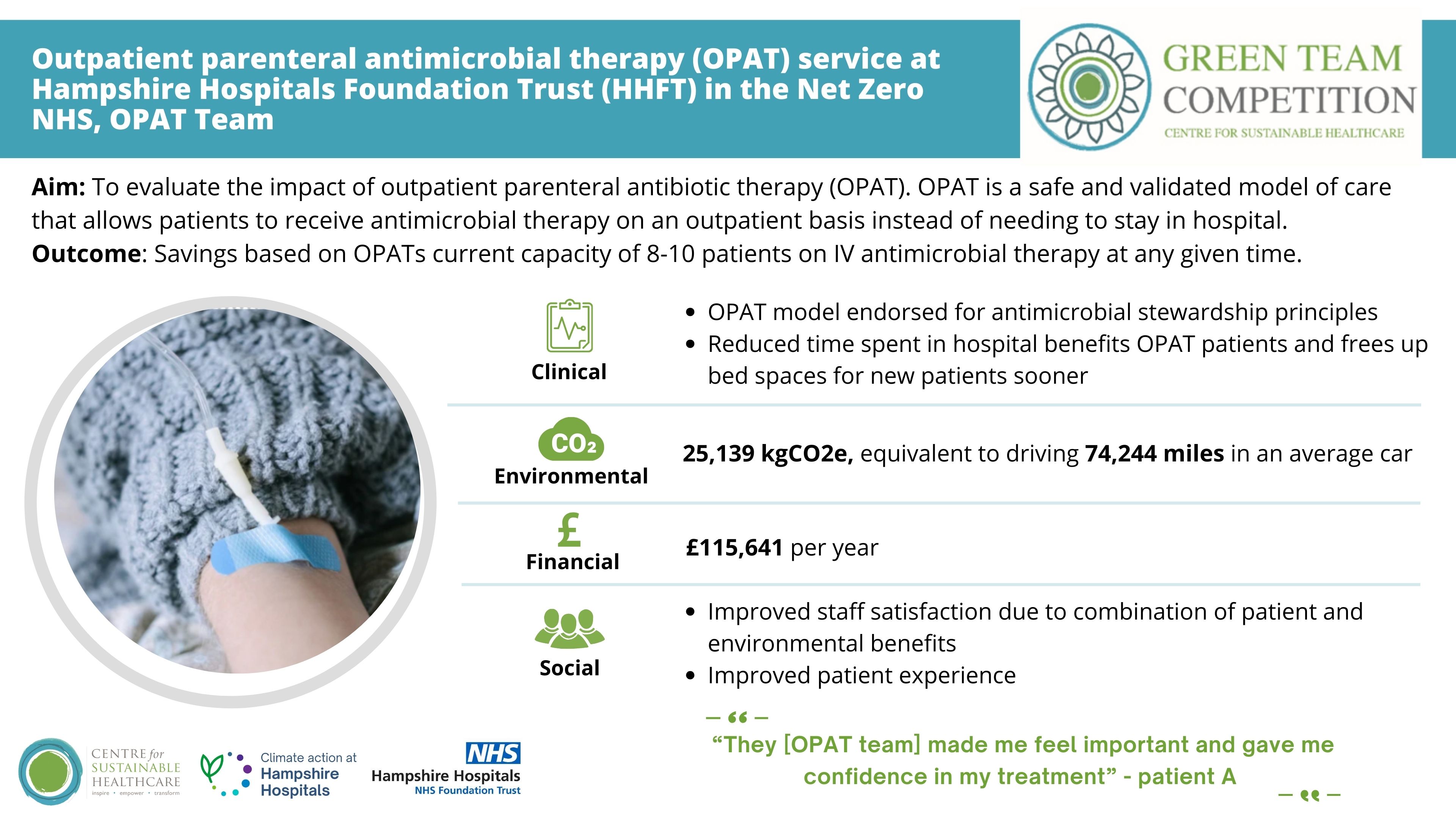
Summary: Outpatient parenteral antibiotic therapy (OPAT) is a safe and validated model of care that allows patients to receive antimicrobial therapy on an outpatient basis instead of needing to stay in hospital for the duration of a medication course.
This competition allowed the team to think about our visibility and accessibility as a service within the trust and ways engagement can be improved going forward. Currently, OPAT is open to any eligible patient across HHFT at BNHH and RHCH sites. Eligibility criteria are clearly defined within best practice guidelines (8). Following formal referral, each patient has an ID/Micro Consultant and OPAT nurse specialist review. This is done in conjunction with the patient in the context of their wider social setting. At present, just over 50% of OPAT referrals received in the trust come from the orthopaedic department. This means a proportion of eligible patients suitable for the service are not being referred.
Team members: J Mazurek, Foundation Year 2 Doctor; J Cunningham, Clinical Lead for OPAT plus /Infection Consultant; R Johnson, Operations Manager for OPAT plus; S Munro, Cellular Pathology Operational Manager; C Mendes, OPAT plus Sister; A Okubuike, OPAT plus Band 6; N Parker, OPAT plus/antimicrobial pharmacist; U Onyendoro, OPAT plus/antimicrobial pharmacist; J Nops, Clinical Services Matron, Community Nursing Team; F Creese, Team Matron Winchester Community Team; B Rogers, Infection Consultant; C Thomas, Infection Consultant
Aim: to evaluate the social, environmental, and financial impact of the OPAT service and to increase engagement and visibility of the OPAT service to the clinical teams across HHFT to encourage appropriate referrals from a wider variety of treating teams.
Method and impact: Using data from existing and previous OPAT patients between December 2022 and August 2023 the team has estimated the average financial and CO2e savings from the different OPAT Pathways compared to ‘standard’ practice involving inpatient admission for intravenous antibiotic therapy.
Clinical and non-clinical staff working within OPAT have been heavily involved in promoting the service amongst the wider medical clinical teams to increase visibility and engagement with the service. Unfortunately, it was not possible to obtain statistics for the engagement this has generated within this 10-week competition period. It was also identified that OPAT can currently safely deliver care for 8-10 patients on IV antimicrobial therapy at any given time– it is effectively working at its full capacity at time of this competition. This presents a barrier to expand until there are means to increase the capacity of the service itself. This remains an area of future improvement and development to maintain long lasting effects and to increase the impact of the OPAT service.
At its current capacity, the OPAT service is demonstrating impressive annual savings of £115,641 and 5,139 kgCO2e, equivalent to driving 74,244 miles in an average car. The service also brings a range of positive benefits to staff and patients.
Summary: The operating theatre environment is a resource intensive area of the NHS with a high demand for specialist medical equipment and single use items.
The Intercollegiate Green Theatre Checklist (2022) has made the recommendation to switch to remanufactured medical devices. A Harmonic scalpel is a laparoscopic surgical instrument that uses ultrasonic vibrations to simultaneously cut and cauterise tissue. In July 2022, the team began to send these devices for remanufacturing via a company called Vanguard, for which we have been reimbursed £5 per device. However, the team were not purchasing remanufactured scalpels for use in their department.
Across our theatre departments at HHFT, a high volume of surgical gowns are used annually, with multiple gowns used for every surgical case. As a trust we have already begun to explore reusable gowns in our theatre department and a trial of these has already taken place prior to the Green Team competition. We aim to make further progress towards full implementation of reusable gowns into our department during the project.
Team members: Laura Vale, Senior Operating Department Practitioner; Krithea Baker, Recovery Nurse Practitioner; Gemma Beckett, Clinical and Operational Lead
Aims: to calculate the environmental, financial and social impact of using a remanufactured Harmonic scalpel versus a new device. And to alculate the environmental, financial and social impact of using reusable versus disposable surgical gowns.
Method and impact: Prior to implementing any changes, the team identified stakeholders they needed to engage and gain support from for both aims. They found that the most important factor was to gather research and make contact with others that had implemented similar projects. Their experience was invaluable to them in getting the project off the ground and helping to resolve issues.
- Harmonic scalpels: the team identified which surgeries would use the harmonic scalpel of which they found they would predominantly be used in laparoscopic gynaecology and colorectal surgery. Specifically this appeared to mainly be laparoscopic hysterectomy and bowel resection and so they decided to focus our trial in these theatres.
Projected across a year an anticipated £50,163 and 395 kgCO2e will be saved (based on purchasing a 67:33 ratio of remanufactured/new scalpel). Staff couldn’t tell the difference between new and remanufactured harmonic scalpel and there will be no negative impacts for patient care. - Gowns: due to price negotiations between the manufacturing company and procurement it wasn't possible to implement the use of the reusable surgical gowns within the project time. Negotiations are recently complete and we predict implementation to start soon. All measurements and results are therefore based on the previous trialling of the product alongside projections.
Projected across a year, gowns will save a projected £23,310 and 52,524 kgCO2e per year. 98.6% staff found reusable gowns clinically acceptable and found more comfortable
Overall, the project has had a positive impact on staff morale and raising awareness of sustainable action that can be taken.
4. HHFT Glove Use Awareness Campaign, Infection prevention and control team
Summary: There was substantial growth in PPE items distributed to health and social care services in England during the Covid19 pandemic, increasing from 2.43 billion in 2019 to 8.7 billion items in 2020. At Hampshire Hospitals, we currently use approximately 276,25 gloves per week (data obtained from the trust procurement department). Projected over a period of twelve months the Trust will use over 13 million pairs.
While gloves are vital pieces of PPE when used correctly, many studies highlight the misuse of non-sterile gloves can increase risk of cross contamination and infection. Inappropriate glove use can also lead to poorer hand washing and hygiene practices.
As an Infection Control team, they feel strongly responsible about the increased glove use within HHFT post pandemic, and used the competition to take action to reduce usage. Tackling the issue of unnecessary glove use now is also financially beneficial as the government support for free PPE will end by 31 March 2024.
Team members: Paula Collinson - Infection Prevention and Control Nurse; Jason Villar - Infection Prevention and Control Nurse
Short term aim: to reduce unnecessary glove use within selected sites by 50% by the end of the sustainability project.
Method and impact:
- Leadership engagement: Ward sisters are key staff to disseminate messages. The team approached and spoke to ward sisters personally about the campaign, highlighting a key message: care, cost, carbon. They encouraged staff to think about the triple benefit to reducing glove use, explaining how reducing glove use is beneficial for patient care, while bringing environmental and financial savings at the same time. They also calculated the potential savings on each ward if glove use was reduced by 50%, and shared these figures with staff.
- No Risk, No Glove Posters: These were placed strategically in areas where gloves are stored on wards to remind staff to consider if gloves are required for the task they were about to do.
- Glove use video: the team is collaborating with the Trust comms team to develop a glove use video to be disseminated trust wide. This video explains:
- The common reasons for inappropriate glove use in the observed wards
- The care, cost, carbon message and benefits
- Uses the phrase “If it’s wet, sticky, and not yours, wear gloves. If not, clean your hands. You do not have to wear gloves all the time” as a reminder for staff to reconsider glove use.
Across 2 trial wards, a 7% reduction in unnecessary glove use was observed. Projected across a year, the project will achieve savings of £992 and 804 kgCO2e, equivalent to driving 2,374 miles.
This project has been valuable for opening conversations between the IPC team and ward teams. As their social survey has shown, there are very mixed opinions on glove use and therefore clear, careful communication is extremely important. Some staff perceived the project was being implemented to take gloves away from clinical teams, and so these concerns need to be addressed.
Long term aim: The team is working with the Trust communications team to develop a Trust wide awareness video to support staff to understand the key reasons for why glove overuse is harmful (including for patients and infection rates) using our care, cost, and carbon messaging.
5. Reducing low value activity in the emergency department, Emergency team
Summary: Operational pressures in the Emergency department mean that in order to aid decision making and prevent delays further down the pathway, ‘just in case’ tests may be taken on arrival to support patient flow and timely care. Unnecessary tests contribute to environmental impact through carbon footprint of the consumables, transport of those consumables, processing of tests and in waste disposal.
Team members: Emma Christmas & Sarah Noble – Consultants in Emergency Medicine; Blessing Zamba – Emergency department (ED) Senior Health Officer; Emily Axford – ED Physicians Associate; Simon Whitehead – Consultant Clinical Biochemist, Clinical Lead for Biochemistry
Aim: to reduce the number of unnecessary coagulation samples in both Basingstoke and Winchester Emergency Departments to reduce consumable waste and reduce carbon footprint.
Method and impact: the team worked with the lab teams to develop baseline data on numbers of samples. They coupled this with sample notes reviews on appropriateness of test. The team calculated potential inappropriate sample numbers and percentage amd used this data as a driver for clinical staff in discussions, education and communications approach.
The Emergemcy team worked to understand barriers to more accurate decision making on whether to take coagulation samples and, on realising that the parameters were actually poorly defined and often left to clinical acumen, developed more specific guidelines for when a sample is indicated to empower and give confidence to nursing staff involved in the initial contact and taking of tests. This underwent multiple PDSA cycles as various clinical input was given from not only Emergency Medicine but also Gastroenterology and Obstetrics and Gynaecology teams.
The team observed a reduction in 1,884 coagulation samples in two months. This is a 24% reduction in coagulation samples (31.4 samples/day). Assuming a similar number can be reduced across the year, 11,461 samples will be saved. It is likely this could be improved upon further, with greater numbers of samples prevented. This reduction equates to a saving of £7,266 and 1,095.67 kgCO2e per year, equivalent to driving 3,236 miles in an average car. With 170 Type 1 EDs in the country, the potential for relatively quickly replicable interventions would yield significant upscaled impact.
This is a saving of 40.11L of blood. Approximately 955 hours (40 days) of lab processing time will also be saved per year. This resource is now available to the wider population and can contribute to faster turnaround of other tests and job satisfaction for the lab team.
Whilst hard to measure, supporting and empowering staff to deliver better care supports a culture where staff take pride in their work and strive to be the best we can be for patients. The benefit of this project has also sparked interest in GreenED as a concept and the following projects are also underway.
6. Reducing The Amount of Wasted Food in Hampshire Hospitals Foundation Trust, Catering team
Summary: Previous food waste data showed that Basingstoke and North Hampshire Hospital (BNHH) and the Royal Hampshire County Hospital (RHCH) in Winchester, collectively wasted ~231 tonnes of food in the 2021/2022 financial year.
Other Trusts have successfully reduced food waste by £100,000 per year, a saving equivalent to 3.53% of the Trusts annual non-pay budget for catering. Our catering team in Hampshire saw an opportunity to achieve the same savings, while minimising our environmental impact.
Team members: Robert Strachan, Head of catering; James Freeburn, Catering Administration Lead; Teri Hope, Facilities Admin Lead; Daniel Freeman, Head Chef; Daniel Ellston, Chef
Aim: to reduce food waste across HHFT, and in doing so:
- saving £100,000 per year
- saving 100 Tonnes of CO2e per year
- saving 500,000 pieces of plastic packaging per year
- adding nutritional value to our patient meals
Method and impact: The team engaged clinical staff to provide information on their perceptions for why food may be wasted (particularly in the areas of untouched meals and plate waste). ‘Just in case’ meals, ordering cut off times, portion sizes, number of courses and meal options were all identified as potential issues. The staff survey stated that one of the main reasons for food waste was loss of appetite whilst in hospital. Smaller portions were identified as a potential supportive factor for encouraging patients to eat.
The team implemented several changes:
- Portion size options
- Reduced number of courses available on the daily menu (additional food is available to patients who would like more)
- Have switched individually packaged items (e.g. cereal, juice) to bulk items
- New menu with more sustainable meat options (e.g. avoiding red meat) and reduced meat, with more vegetarian and vegan options
- Vegetable sides were amended to include more locally grown, in season ingredients
- High waste dishes (scrambled eggs) removed
- New moulded IDDSI meals (specialist texture meals) that look at taste better
- Where possible unnecessary packaging has been removed, while remaining packaging has been exchanged to paper, starch or bio-plastics.
A mealtime manifesto has been produced to promote best ward practice and create a positive environment for patients during meal times. While this has been produced as part of the project it was not widely dispersed during the measurement period.
Trust wide, the team have projected annual savings of £157,135 and 143,716 kgCO2e per year, equivalent to driving 424,442 miles in an average car, roughly 17 times around the circumference of the Earth. There will be a smaller additional saving for reduced food waste disposal (estimated at approximately 115 kgCO2e and £4,984 per year).
Socially, the team have raised awareness of links between food and environment within the catering team. The project also addressed concerns from staff and patient on reasons for why patients may not eat meals (e.g., portion sizes). Feedback from patients has been extremely positive.
Plate waste has reduced significantly, which is due to a combination of reduced food given on the trays, and patients eating more of the food they receive. One third (32%) of people in the UK aged 65 years or over are at risk of malnutrition on admission to hospital and so providing nutritious, appealing meals is important. The team observed that at the time of their menu change, mean length of patient stay reduced. While unlikely to be the only contributing factor, menu changes may have enhanced patient recovery.
Awards
 Congratulations to the winning team, Catering!
Congratulations to the winning team, Catering!
The project team were praised by the judges for their engagement of clinical staff and patients to identify suitable changes and drive improvement alongside the catering department. This has led to significant environmental and financial savings, while optimising patient care and experience.
"The Green Team Competition is a brilliant initiative which captured the energy and enthusiasm of our frontline teams from across the Trust. The projects saved carbon, saved money and improved patient care. They really showcased some of the outstanding innovation in our teams. The judging was incredibly difficult as every project was a winner!” Alex Whitfield, Chief Executive
The Centre for Sustainable Healthcare would like to thank and congratulate all teams that took part in the competition. The competition's outcomes serve as proof of the teams' commitment and efforts to improving the sustainability of the healthcare system.
Acknowledgments
CSH would like to thank our 6 Green Teams for their enthusiasm, dedication and creativity in devising and completing their projects.
Gillian Brown, Head of Sustainability; Miranda Chubb, Energy and Sustainability Officer and Yvonne McWean, Associate Director Quality Improvement for partnering with us in the competition and supporting the teams.
The judging panel for your time, thoughtful questions and encouraging comments:
- Alex Whitfield, Chief Executive, HHFT
- Shirlene Oh, Chief Strategy and Population Health Officer, HHFT
- Tamara Everington, AMD for Change, HHFT
- Louise Fox, Associate Director Nursing, HHFT
- Rachael Ward, Networks Lead, The Centre for Sustainable Healthcare
Thank you to Rosie Hillson – Environmental Analyst (CSH) for her careful and highly skilled work in carbon footprinting. Rosie supported the teams in carrying out their own carbon footprinting and equipped teams with the knowledge and tools to carry out future calculations for projects in the future. Carbon calculations are essential to integrated project reporting and make plain the true cost and impacts of services to allow better, safer and more responsible decisions to be made in healthcare organisations.

