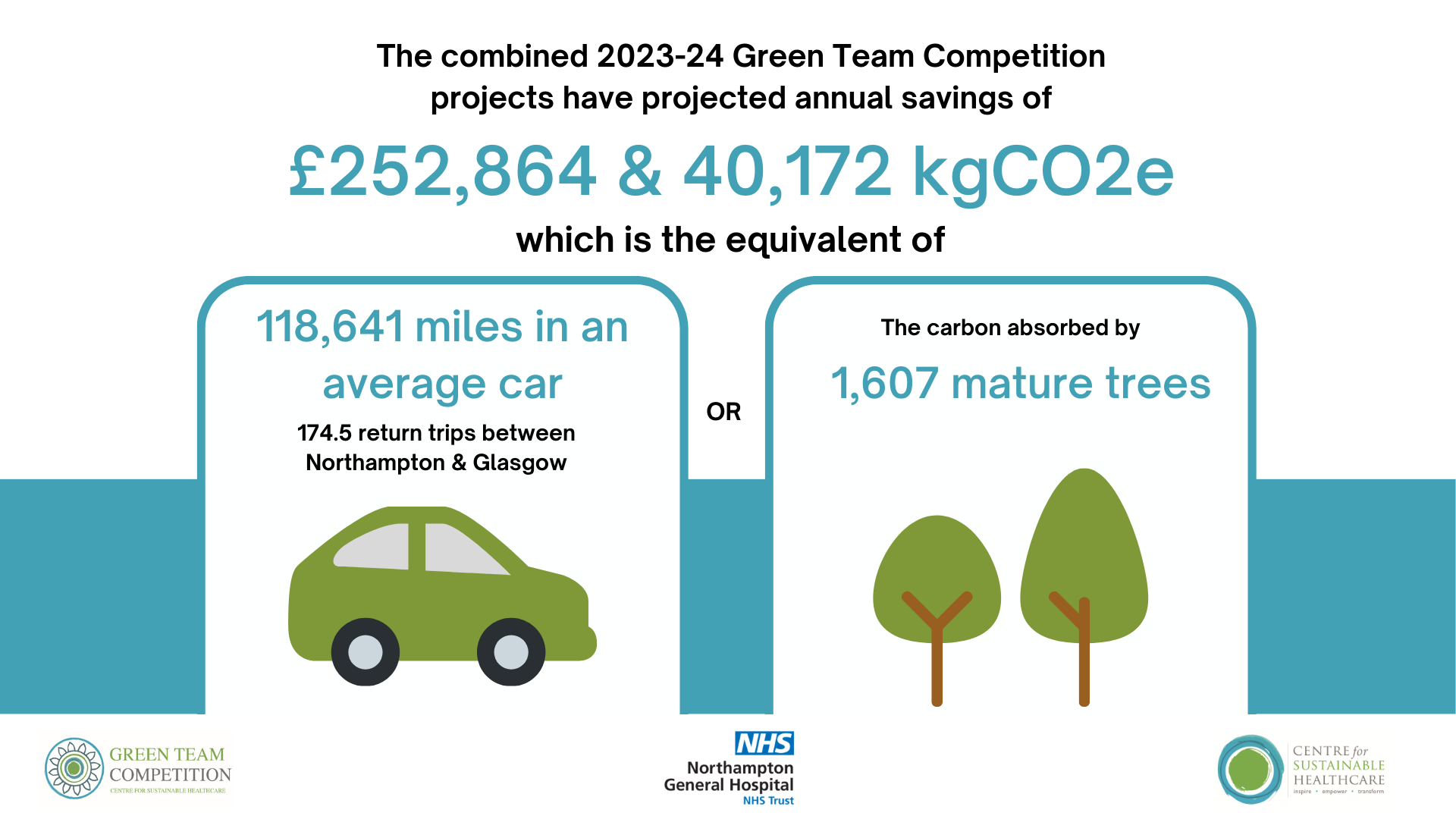
Northampton General Hospital NHS Trust Green Team Competition expected to save £252,864 & 40,172 kgCO2e annually
In September 2023, Northampton General Hospital (NGH) NHS Trust commenced a Green Team Competition in partnership with the Centre for Sustainable Healthcare. The competition has brought anticipated annual savings to the Trust of £252,864 & 40,172 kgCO2e. This is the carbon footprint equivalent of driving 118,641 miles in an average car (or 174.5 return trips between Northampton & Glasgow).
Clare Topping, Head of Sustainability, said:
"This is the second time we have taken part in the Green Team Competition and we have seen some amazing entries and evidence of improved sustainability and patient outcomes. It gives our colleagues, no matter what their role, an opportunity to have support in trying new ideas and to take ownership of leading change. Many of the ideas have wider benefits too and are shared with other hospitals and healthcare providers locally, nationally and internationally.
As a hospital it's our responsibility to look after our local community, and that includes a responsibility to look after our environment and manage our too. By running the competition we can encourage and champion change for Northampton and beyond."
Through the Green Team Competition, six teams from NGH were selected to engage in our award-winning programme in sustainability in quality improvement (SusQI) that transforms expert knowledge into action. Each team received mentoring from CSH facilitators to drive healthcare transformation by developing, implementing and measuring the impact of projects through the lens of the sustainable value equation.
 At the March 7th Showcase and Awards Ceremony, the teams presented their projects, including the anticipated savings and opportunities to scale and spread, to an audience from the Trust and the judging panel including:
At the March 7th Showcase and Awards Ceremony, the teams presented their projects, including the anticipated savings and opportunities to scale and spread, to an audience from the Trust and the judging panel including:
- Nerea Odongo, Director of Nursing
- Paul Slater Clinical Director Anaesthesia
- Paul Shead Director of Estates and Facilities
- Palmer Winstanley Chief Executive Officer
- Hazel Walsh, Clinical Transformation Programme Manager, The Centre for Sustainable Healthcare
Nerea Odongo, Director of Nursing said “If you create opportunities where people can have simple ideas, the impact we can have on our patients is huge”.
Awards
Palmer Winstanley, Chief Executive Officer who announced the award said “It’s a real privilege. Thank you for your efforts on top of your incredibly busy jobs - you should be proud of what you are doing”.
 Winners: Hand Therapy team
Winners: Hand Therapy team
Congratulations to the WINNING team, the Hand Therapy team, led by Lucy Wimmer and Emma Baker. Their project was a simple pathway change that led to better patient outcomes while saving significant staff time across the MDT. The project is an excellent example of how better clinical care is more sustainable care.
Highly commended: FIT Shared Decision-Making Council
Special mention to: Endoscopy team
The Centre for Sustainable Healthcare would like to thank and congratulate all teams that took part in the competition. The competition's outcomes serve as proof of the teams' commitment and efforts to improving the sustainability of the healthcare system.
“This QI project widened my consideration to how process changes can not only benefit patient care but also have sustainable benefits. I was so surprised and pleased that such small changes could have a big impact. Protecting our environment is very important to me and I am keen to support the NHS on their carbon neutral pledge. I look forward to our next project!“
Lucy Wimmer, Hand Therapy Team Lead
“We learned a lot about sustainability while undertaking this project, small changes really can make a big impact. The competition was challenging but ultimately very rewarding and we received so much support and encouragement along the way”.
Emma Baker, Hand Therapy Team Lead
Most of the projects not only have the environmental benefits of saving CO2e, reducing waste, and ensuring future healthcare sustainability, but they also improve outcomes and patient experience. For the winning idea this year our Hand Therapy Team changed the care pathway for patients, meaning they reduced the number of appointments patients had to attend, reduced the amount of time until patients had full function back, saved staff time, and reduced carbon emissions and waste as well as having a significant financial benefit.
Clare Topping, Head of Sustainability
Green Team Competition Projects
Read the full Impact Report here or view the project summaries below.
- Hand Therapy Pre-operative Appointment for Plastic Hand Trauma Patients, Hand Therapy
- Have Confidence with Continence, Falls, Infection Prevention & Control and Tissue Viability (FIT) shared decision making council
- Bowel Preparation for Colonoscopy, Endoscopy
- Reducing travel for blood tests used for Radiotherapy Planning, Radiotherapy
- Staff education on appropriate medicines waste segregation & use of patient’s own medicines, Renal Specialist Pharmacy
- A paradigm change: from disposable to reusable instruments usage in the Ophthalmology Department, Ophthalmology
1. Hand Therapy Pre-operative Appointment for Plastic Hand Trauma Patients, Hand Therapy
Team members: Emma Baker and Lucy Wimmer, Hand Therapy Team Leads
Setting / patent group: Hand therapy outpatient department
Issue
Hand Therapy is an outpatient department accepting acute referrals from trauma and orthopaedics (T&O) consultants, Virtual fracture clinic and Plastics consultants. The department works closely with both these specialties and run joint MDT clinics.
All postoperative patients are required to be seen in hand therapy 3-5 post op as per British Association of Hand Therapy Guidelines. This can be challenging to find appointments at short notice and to make successful telephone contact with the patient to inform them of their appointment. If the team is unable to contact a patient via telephone this results in a delay to care as extra time is required for sending out appointment letters which the trust sends 2nd class. It has been noticed anecdotally that these patients have increased complications and require higher hand therapy input as a result. There is evidence to suggest early hand therapy and good patient education can reduce complications and improve patient compliance.
Intervention
Hand therapy often need to see patients on the 3rd day post op, it was previously hard to get quick enough appointments. Patients had little to no information regarding what to expect of Hand Therapy and the timescales required. Hand Therapy admin team were often challenged by patient that their appointment was too soon as they still had postoperative Plaster of Paris or bandage in situ.
The Hand Therapy Team Leads streamlined this process by creating a new pathway. This was discussed with plastics consultants and registrars for their approval. The process was disseminated to the wider Hand Therapy Team and communicated to the Therapies manager. In the new pathway, patients identified as needing surgery are sent straight from their plastics appointment to the hand therapy department. A hand therapist sees patient when able (usually within 15 mins) to:
- discuss the hand therapy process with patient and answer questions
- provide handout including general post op information and Hand Therapy contact details
- complete Quick DASH outcome measure
- discusse complications
- schedule hand therapy appointment for 3-5 days post op where possible
The plastics team complete a hand therapy referral and no further action is needed until the patients first appointment 3 days post op.
Outcomes
The team has compared outcomes for 10 patients on each pathway, with the below savings projected annually.
Patients: The number of patient appointments reduced as well as duration under hand therapy (by 21.2%) and consultant care. There was a reduction in delayed care and patient satisfaction was maintained/ slightly elevated generally throughout the service. The team received good feedback verbally from the consultants and improved communication and confidence between departments. Patient expressed verbally that they felt a sense of confidence that they knew the plan going forward, and physically where to come to for their appointment which helped to reduce stress and anxiety.
Environmental savings: For 10 patient episodes of care they observed a reduction in 33 appointments with the consultant team (726 kgCO2e) and a reduction in 45 appointments with the hand therapy team (990 kgCO2e). This is an average saving of 171.6 kgCO2e per patient. With an average of 11 post op plastics patients referred into the service per month, the team anticipates annual savings of 22,651.2 kgCO2e, equivalent to driving 66,896 miles in an average car.
Financial savings: A reduction in 33 consultant appointments saves £6,072 from 10 patient episodes of care. Projected across the year to full caseload, this is £80,150. A reduction in 45 hand therapy appointments equates to £618.75 from 10 patient episodes of care. Projected across the year to full caseload, this is a saving of £8,168.
DNA cost savings: The team has conservatively estimated they can prevent 1 DNA per month, a saving of £165 a year. A 43% decrease in stock cost for the HT team was seen equating to £26.45 (£2.65 per patient). Projected across a year this equates to £349. In total the projected annual savings from the project are £88,829.
Patient comments:
"Everyone should be aware of environmental impact. Any effort to be sustainable is a good effort”
“We all have to do our best to minimise carbon footprint, hope the therapy unit can do this too”
Staff comments:
"I found it really improves patient pathway and improves admin systems and it reduces patient anxiety (Hand Therapy)”
“I think it is so much quicker and it has saved me a lot of work and I appreciate the change in the system (Admin)”
“Thank you, this is excellent work. My appraiser was very impressed with the results of the audit, he has recommended that you register this audit with the trust quality and effectiveness group (Consultant)”
Key learning point
The team found that good communication between staff members and teams was key to the success of the project. Positive feedback from staff and patients was a motivating factor to continue and succeed with this project. Overall attitudes to the project have been positive because the multiple benefits have been apparent.

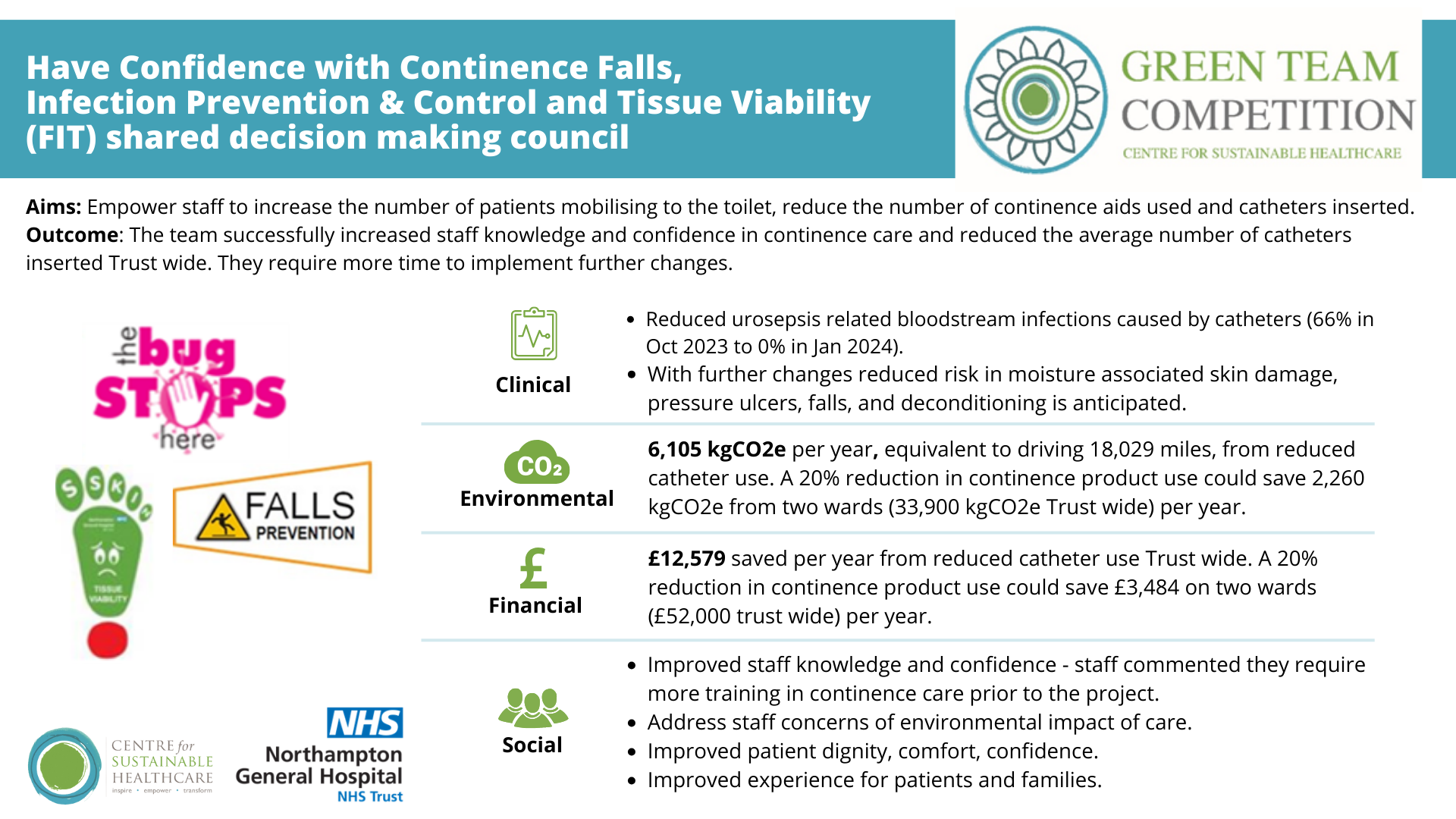
Team members: Holly Slyne - Assistant director infection prevention and control (IPC); Ros Pound - IPC Matron; Natalie Clews - IPC Clinical Nurse Specialist; Elizabeth Lomax-Enfield - Falls prevention coordinator; Janet Jousiffe -Deputy falls prevention coordinator; Lystra Cunningham -Tissue viability specialist nurse; Jade Moss -Tissue viability specialist nurse; Sara Hollis -Tissue viability specialist nurse
With Recognition of support with great thanks to Continence product information support from procurement team, local company representatives of products used and trial assessment ward staff.
The Falls Prevention, Infection Prevention and Control (IPC) and Tissue Viability Shared Decision-Making Council was created 6 years ago as a collaboration to work in a proactive way to make a sustainable change by protecting our patients from harm from falls, pressure ulcers and infections at the same time as there were commonalities of challenges. One area in which their work commonly overlaps is in relation to continence care, with a focus on patient well-being and the prevention of complications. Clinical continence care generates a significant amount of waste and continence pads take 500 years to biodegrade, so we are keen to implement initiatives to reduce this waste and decarbonise care processes.
Setting / patent group: two trial ward where continence care related issues were reported, focussing on patients over age of 65. some changes made Trust wide.
Issue
Poor continence management can have significant implications, including an increased risk of sacral pressure ulcers due to improperly fitting products leading to leaks and prolonged exposure of the skin to urine or fecal matter. This exposure can compromise skin integrity, leading to various skin conditions and infections. Additionally, reliance on containment strategies such as pads for individuals who could otherwise walk to the toilet contributes to distress and loss of dignity, creating unnecessary work for staff. Moreover, poor continence management can lead to complications such as catheter-associated urinary tract infections (UTIs) and an increased risk of inpatient falls due to prolonged periods of inactivity, which can result in deconditioning. At NGH, there is a focus on individualized assessment and care to promote mobility, independence, and prevent falls, but there is a concern regarding the provision of poorly fitting or unnecessary continence products, which can further exacerbate these issues. Addressing these concerns through optimized continence care is crucial for patient well-being and reducing associated financial and environmental costs.
They engagement with staff who provide continence care, several problems were identified:
- Lack of individualised continence assessment and documentation:
- not all patients received a full assessment to ascertain their individual need as no care plan for continence was in place, only for incontinence and catheter care
- continence care was mostly recorded on care rounding care plans, input /output charts and stool charts if required for that patient - Lack of awareness of wider impact of continence care:
- not all staff were aware of connections to continence care and deconditioning, fatigue relating to admitting condition, comorbidities and length of stay, and how promoting continence can also promote functional physical activity - Lack of staff confidence:
- from the survey results, staff were not confident in measuring and selecting appropriate continence products
- many staff requested further training - Incorrect stock on wards:
- wards did not have the correct / most appropriate items ordered or a correct range of items to make appropriate choices. Without the correct options, and with limited capacity, staff need to make do with what is available at the time
- wards did not have barrier creams on regular order process
- no appropriate items for “just in case” requirements. For example, staff commented that for a patient that wants a small pad just in case of urgency incontinence while they get used to the ward and where the toilet is had to be given a very large pad as there was no other options - Incorrect sizing of continence products:
- patients were being given inappropriate products, likely due to a combination of stock availability and staff confidence.
Intervention
The team aimed to:
- reduce the number of continence aids used in 2 elderly medical wards in the Trust by 20% by January 2024
- increase the number of patients mobilising to the toilet in 2 elderly medical wards
- reduce the number of moisture associated skin damage, pressure ulcers and falls in 2 elderly medical wards
- reduce the number of urinary catheters in situ in 2 elderly medical wards, and further across the Trust
- increase staff knowledge on continence products
- increase the patient experience of being in hospital and maintaining continence
They implemented the following changes:
Confident Continence half day study day where company representatives provided training on the barrier creams, how to select the correct pad, how to measure a patient correctly for pants. TVNs provided training on how to prevent moisture associated skin damage, IPC nurses provided training on catheter prevention strategies and the Falls Prevention Team provided training on mobilising patients out to the toilet safely.
A guideline for catheter avoidance and appropriate selection of continence products was written by IPC Team and the IPC team conducted weekly catheter prevention ward rounds to teach staff, prompt removal and prevent catheter insertions. This also included teaching staff about the barrier creams and correct use of incontinence aids. The Team decided to launch this Trustwide rather than on the 2 pilot wards as it was easier to implement and measure on a wider scale through the electronic VitalPAC system.
Changes planned / Next steps
Unfortunately, winter operational pressures and a delay in different sizing of continence products arriving to NGH had an impact on the pace of this project. Therefore, the following changes are scheduled to take place in the coming months
- Provision of small pads and pants to trial wards
- An Out to Toilet training initiative will commence in March. This will involve a pop up video on the Trust Facebook page showing how to safely walk patients to the toilet and supportive visits from the FIT Team to wards to reinforce it and ensure staff are walking patients to the toilet. Weekly data collection of number of patients mobilising will be collected. The FIT team have recruited 2 new voluntary team members from the IPC Team who can support the pilot. They will then trial for 2-3 months on the two trial wards before evaluating the impact and potentially expanding the pilot wider
Outcomes
Clinical: Reduced urosepsis related bloodstream infections caused by catheters (66% in Oct 2023 to 0% in Jan 2024. With further changes reduced risk in moisture associated skin damage, pressure ulcers, falls and deconditioning is anticipated.
Environmental: 6,105 kgCO2e, equivalent to driving 18,029 miles from reduced catheter use. A 20% reduction in continence product use could save 2,260 kgCO2e from two wards (33,900 kgCO2e Trust wide).
Financial: £12,579 saved annually from reduced catheter use Trust wide. A 20% reduction in continence product use could save £3,484 on two wards (£52,000 trust wide) per year.
Social:
- Improved staff knowledge and confidence - staff commented they require more training in continence care prior to the project
- Address staff concerns of environmental impact of care
- Improved patient dignity, comfort, confidence
- Improved experience for patients and families.
Key learning point
Through this project the team has identified that optimal continence care encompasses a much wider range inter-related issues than first realised. Staff engagement from their Confidence Continence Day was key to success of this project. Staff were very willing to attend and take part in surveys and conversations while being open about their knowledge and confidence. The team learned valuable information on why staff find it challenging to optimise their care, to best inform our changes. Showing multiple benefits for patients, costs and the environment was supportive for motivating staff to change practice.
3. Bowel Preparation for Colonoscopy, Endoscopy
Team members: Sue Broughall - Endoscopy Compliance manager; Theresa Passmore - Endoscopy Manager; Patricia Ojo - Endoscopy Junior Sister
Setting / patent group: Endoscopy
Issue
The quality of bowel preparation pre-endoscopy is crucial because inadequate or incomplete bowel preparation can lower screening effectiveness and increase health care expenses due to longer or aborted procedures. The Endoscopy service has historically prescribed Moviprep, requiring a patient to drink 2 litres of a laxative solution that has a poor taste. Patients would be required to drink an additional 2 litres of water, making a total of 4 litres of fluid. It was therefore a concern that some patients attend for colonoscopy and have their procedure abandoned, cancelled on the day and rebooked due to poor bowel prep while some will not attend citing inability to tolerate high volume bowel preparation and poor taste.
Intervention
A novel low-volume bowel preparation regimen, Plenvu (Norgine) is polyethylene glycol [PEG] laxative designed for oral bowel preparation use before an elective colonoscopy procedure in adults. Plenvu can be administered in 1 litre, as a 1 day or 2 day regimen has recently emerged. This could offer the potential for enhanced compliance and potentially improved bowel preparation outcomes. A recent (2021) study in London demonstrates that Plenvu is a low volume (1 litre) polyethylene glycol (PEG) plus ascorbate-based bowel preparation which has demonstrated a superior cleansing and equal safety and tolerability profile compared with standard agents (7). Plenvu met the low volume, effective, palatability and convenience criteria on the Boston Bowel Preparation Scale (BBPS) scores.
Outcomes
The team has switched to routine use of Plenvu in 90% cases. While their service has a low rate of failed colonoscopies (2.7%) exceeding UK JAG performance indicators, they hope to see further reductions in failed procedures over the coming 12 months. The team also hopes to see reduced rates of DNA procedures.
They require 12 months to evaluate the impact of the change, with predicted outcomes below based on an assumption that 59% (78/132) failed colonoscopies, and 50% DNA and cancellations per year can be prevented from this change.
Environmental: Saving of 1,361.5kgCO2e, equivalent to driving 4,027.43 miles in an average car.
Financial: Saving of £29,284.30 per year from switch to Plenvu. Additional income of £72,226 per year from replacing failed procedures and wasted slots from cancellations/DNAs with successful procedures.
Social impact: 62% staff agreed poor bowel prep is a frequent problem in our unit and 50% felt Plenvu would support this problem.
Staff comment “If the prep works right then there would be less patients being rebooked and less waste”
Key learning point
The key elements that contributed to the success and learning in this study is the QI training, support, information resources and organisational process support received and links to patients benefit and clinical outcomes alongside environmental and financial benefits.
4. Reducing travel for blood tests used for Radiotherapy Planning, Radiotherapy
Team members: Rachel Tighe, Therapy Radiographer – (rachel.tighe2@nhs.net); Hayley Hall, Therapy Radiographer (hayley.hall11@nhs.net); Deborah Chapman, Therapy Radiographer; Peter Goldie, Radiotherapy Physicist.
Setting / patent group: Radiotherapy/Oncology
Issue
The Radiotherapy contrast procedure (Radiotherapy, 2023) states that patients should have an estimated glomerular filtration rate (eGFR) of >45ml/min/1.73m² before a contrast scan, and so each patient requires an up-to-date blood test. It was identified that patients who required this test were travelling to the hospital for an additional appointment to have their bloods taken in radiology. This practice had come about from the covid19 pandemic, when radiographers were trained to take bloods, to avoid patients attending blood-taking units, reducing risk of infection. However, this practice was now not the most convenient for patients or staff, and could be prevented with patients a) having bloods taken in at the hospital blood-taking unit on the same day as their consultant appointment or b) having bloods taken at another centre closer to home (if they had a virtual consultant appointment or an appointment more than 30 days before their scan – too early for bloods).
Intervention
The Consultant Clinical Oncologists and clinic-trained radiographers who conduct clinic consultations were engaged. An introductory email to the project aims, baseline findings, proposed changes and benefits was sent. The team requested that all patients who require contrast bloods are sent directly from their clinic consultation to their blood test. At Northampton General Hospital this is possible as Oncology patients are allowed to walk into the blood taking department at any time for a blood test (i.e. don’t need an appointment). The request was re-iterated at Radiotherapy Consultant Meetings.
For patients who will still require travel, the team reviewed local options. As some GPs will not conduct blood tests, they researched local centres and hospitals blood taking policies for different areas of the county, so they had this information available for patients moving forward.
Outcomes
Evironmental: For patients who could have bloods straight after their consultation, the team saved 191.3 miles for the 2-week period, equating to 4,973.8 miles per year or 1,684.1 kgCO2e. If the changes to patients attending more local centres is maintained, they will almost double the annual saving, with an additional 183 miles, or 1,610 kgCO2e saved.
Social:
- Their changes will streamline the patient journey and make blood tests more convenient
- Patients may have small financial savings from reduced travel costs
- Radiotherapy staff will save approximately 27 hours per year from reduced blood taking, which can be redirected to higher value work
Key learning point
The initial learning about SusQI and what area can have the biggest impact helped them focus their research in an area the team had not thought of looking at.
Team members: Janeme Lam, Renal specialist pharmacist; Shelley Rossiter, Renal ward manager
Setting / patent group: Renal ward
Issue
There is a high volume of medication returned to the pharmacy team from the renal ward at Northampton General Hospital. While ward staff are often placing medications in a pharmacy return box, believing any medication sent back to pharmacy can be re-dispensed for another patient. This is not always the case. All patient’s own drugs (PODs) and split packs issued by the hospital cannot be returned to be reused due to health and safety recommendations. There are reasons why hospital-supplied medicines may also be unsuitable to re-dispense. All medicines sent back to the pharmacy need to be segregated by the dispensing team. Suitable medications will be returned into the system for re-dispensing, and others will be incinerated as clinical waste. This is an extremely time-consuming process for pharmacy staff.
Oversupply of patient’s routine medicines can contribute to pharmaceutical waste. Patients may forget to bring in medication they already have at home, or even if their medications are brought in, ward staff may use hospital supplies to ensure the patient has their own medication on discharge. However – prescriptions will often change during admissions meaning the initial medication brought in is no longer appropriate to take home and needs to be incinerated. All patient medications are often requested on discharge, however is a medication has been unchanged during admission, it is likely the patient doesn’t need those medications to be prescribed – which would save dispensing time.
Intervention
- The first aim of this project (Task 1) is to reduce dispensary staff time processing medicines returns by providing nurses education on how to segregate PODs and hospital-supplied medicines into designated medicines return boxes on the ward.
- The second aim (Task 2) is to encourage patients to bring their own routine medicines to hospital to reduce the need for hospital dispensing.
Education was provided to ward and pharmacy staff:
- background of sustainability in healthcare
- how much time dispensary staff are currently spending to process medicinal waste from the pharmacy return box
- the process of segregating PODs and hospital-supplied medicinal waste into the designated medicines containers on the ward
- educating nurses to ask patients to bring in PODs, use PODs during hospital stay instead of using ward stock; return PODs to patients on discharge
- educating pharmacists and pharmacy technicians during the drug history process, to ask patients and their relatives to bring in PODs; for those patients who have brought their medicines to the hospital, to ask patients how much supply they have at home; encourage patients to order PODs from the GP rather than supply from the hospital on discharge; endorse on drug charts that patients can obtain their routine meds from GP
Outcomes
Financial and environmental: On one ward, the combined aims have projected annual savings of £19,680 and 3,435 kgCO2e, equivalent to driving 10,143 miles in an average car.
Social: Socially, 62% of ward staff and 89% pharmacy staff agreed medication waste is a huge problem. Prior to the project dispensing staff expressed frustration at the time spent segregating medications returned from the ward. It is estimates form this project staff will save (2 days) of time in a year for one ward. There are 21 adult wards in NGH. Prior to the project - 100% of pharmacy staff felt there is duplication of dispensing as patients can bring in their medications from home. 50% of ward respondents reported they used patients own medications first rather than ward stock showing room to optimise this.
Two patients were surveyed. Both were concerned about the environmental impact of healthcare. Both stated they will only require new medicines on discharge to reduce medicines waste, obtaining medications they were already taking from the GP.
Clinically, There is no compromise of patient outcomes by implementing this project. Although data has not been collected due to time limitations in the project, some potential impacts include:
- a reduction in medicines omissions, especially critical medicines by encouraging patients to bring in their PODs to be used in the hospital
- discharge medications may be dispensed quicker due to reduction of dispensing items. This will hopefully have a positive patient outcome as patients can go home quicker
Key learning point
The key elements that contributed to the success of the project include good engagement with the ward pharmacist, nurses, and other pharmacy colleagues. From the staff survey, the majority has raised concerns of medicines waste affecting environmental impact and they want to do something about it. The project has shown by breaking down communication barriers and misconception, multidisciplinary team can work efficiently, cost effectively and environmentally friendly.
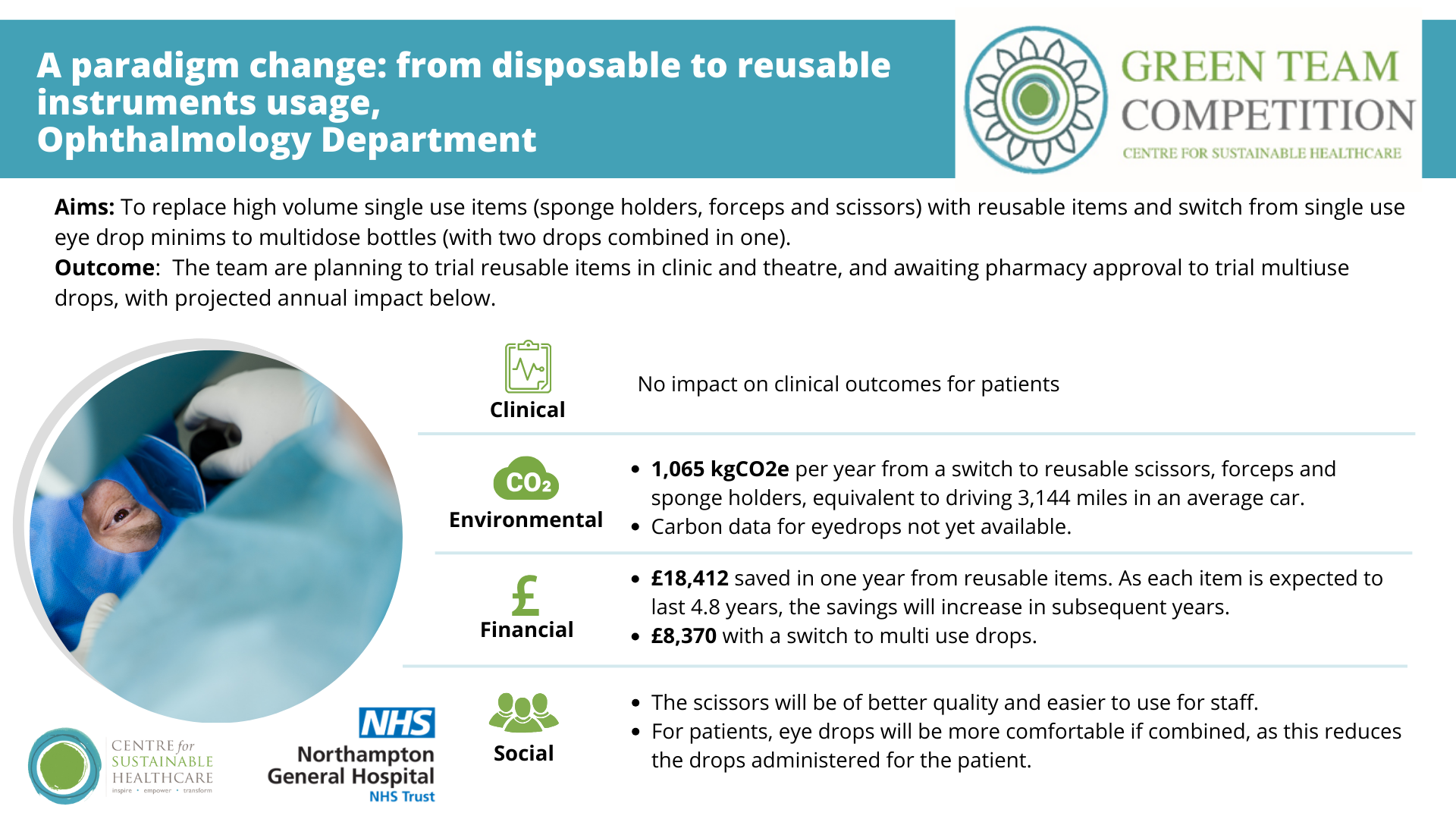
Team members: Tristan McMullan, Consultant ophthalmologist; Gabriele Quaranta, Oculoplastics Fellow
Setting / patent group: Ophthalmology outpatient department, with a patient turnaround of approx. 100-200 patients per day, seeing over 25.000 patients per year.
Issues
- Many procedures in the department use single-use items but could be performed equally well using reusable instruments. While the department has replaced some single use with reusable items in the past, the reusable option has not been optimised. For example, they currently use reusable scissors in our ophthalmology sets, however they are blunt.
- In ophthalmology, they routinely administer/prescribe dilating eye drops (tropicamide). This is administered via single dose minims. There are more sustainable alternatives to minims. By administering drops from multidose bottles that can be used safely with multiple patients they will significantly reduce packaging. Rahemtulla et al 2021 compared annual financial costs between multidose bottles and single-use minims finding use of multidose bottles was $22,481 CAD (approximately £13,250) cheaper than minims in their Department. This is a cost saving but also avoids a huge amount of plastic waste.
Intervention
- To replace high volume single use items (forceps and scissors) with reusable items in clinic
- To replace a high-volume single use item (sponge holders) with reusable in theatres
- To switch from single use eye drop minims to multidose bottles
The team has purchased reusable sponge holders, forceps and scissors. The new forceps will be used in clinic. The sponge holders will be used in theatre sets. The new scissors will be used in theatre sets, replacing our current reusable scissors which are bunt. The worn scissors will be sent to clinic to be used for suture removal as that task is much less demanding than a surgical operation, and blunt scissors will not impact.
They gained infection prevention and control (IPC) approval for the changes, including eye drops. They are awaiting pharmacy approval to trial this change.
The team plans to trial the items and gain feedback from staff before rolling out the changes. In future they would like to replace more disposable items with reusable (e.g. sterile drapes), and spread the changes to other surgical departments.
Outcomes
Clinical: there will be no changes to clinical outcomes for patients. For patients, eye drops will be more comfortable if combined, as this reduces the drops administered for the patient from 2 drops per eye to 1 single drop per eye.
Replacing the scissors in theatre will make operating more pleasant without requiring asking for a new pair of scissors for almost any oculoplastic operation. The reusable scissors will be easier for the team to use as the disposable ones are very sharp and small, therefore not ideal for the kind of procedures that we commonly perform.
Environmental: across a year, they will save 1,065 kgCO2e from a switch to reusable scissors, forceps and sponge holders. This carbon saving is equivalent to driving 3144 miles in an average car. While a switch to multi use drops would bring further carbon savings, they are still collating data to estimate the carbon footprint of a multi-use bottle.
Financial: they will save £18,412 in one year from the switch to reusables. As the reusable items are expected to last for 4.8 years, the savings will increase in subsequent years. Their savings will increase by a further £8,370 with a switch to multi use drops.
Key learning point
The key elements that contributed to successes and learning in this project was the critical evaluation of their practice to understand how they do things and how they can do them in a more environmentally friendly way, maintaining patient safety all the while.
The team learned that they need to be proactive in order to start a change that will then become common and accepted practice, although there can be some resistance initially. Encouraging staff to see this as a common goal rather than a veiled criticism of their current practice is key.