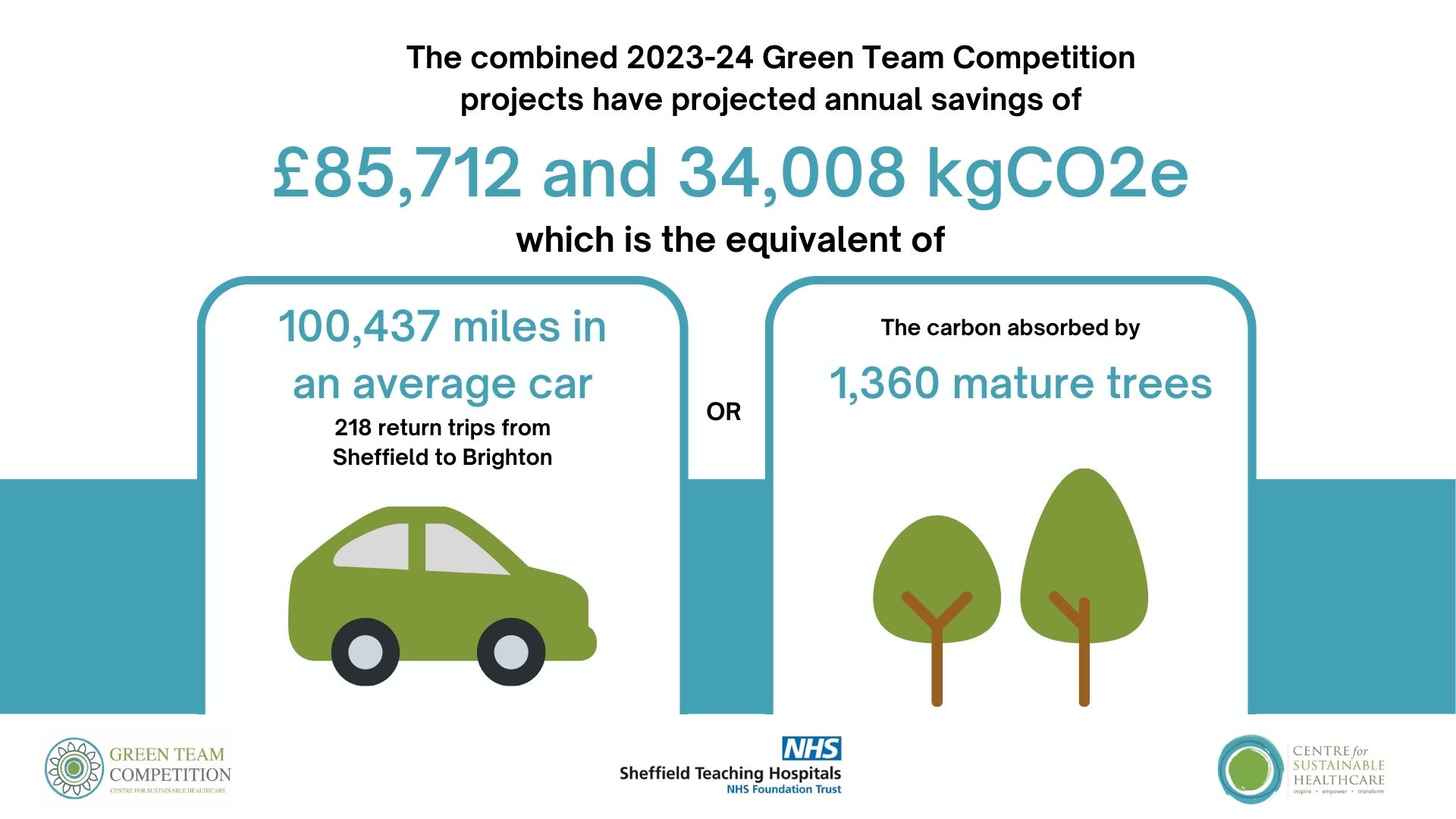
Sheffield Teaching Hospitals NHS Foundation Trust Green Team Competition expected to save £85,712 and 34,008 kgCO2e annually
In September 2023, Sheffield Teaching Hospitals (STH) commenced a Green Team Competition in partnership with the Centre for Sustainable Healthcare. The competition has brought anticipated annual savings to the Trust of £85,712 and 34,008 kgCO2e. This is the carbon footprint equivalent of driving 100,437 miles in an average car (or 218 return trips between Sheffield and Brighton).
Through the Green Team Competition, six teams from STH were selected to engage in our award-winning programme in sustainability in quality improvement (SusQI) that transforms expert knowledge into action. Each team received mentoring from CSH facilitators to drive healthcare transformation by developing, implementing, and measuring the impact of projects through the lens of the sustainable value equation.
At the March 5th Showcase and Awards Ceremony, the teams presented their projects, including the anticipated savings and opportunities to scale and spread, to an audience from the Trust and the judging panel including:
- Charlie Elliot - Deputy Medical Director
- Rachel Morris - Head of Sustainability
- Mark Tucket - Director of Strategy and Planning
- Paul Buckley - Deputy Director of Strategy and Planning
- Cath Richards, SusQI Programme Lead at the Centre for Sustainable Healthcare
Charlie Elliot, Deputy Medical Director, said, “It was a fantastic afternoon hearing about the work being done by so many highly motivated and dedicated people, just a shame there could only be one winner!“
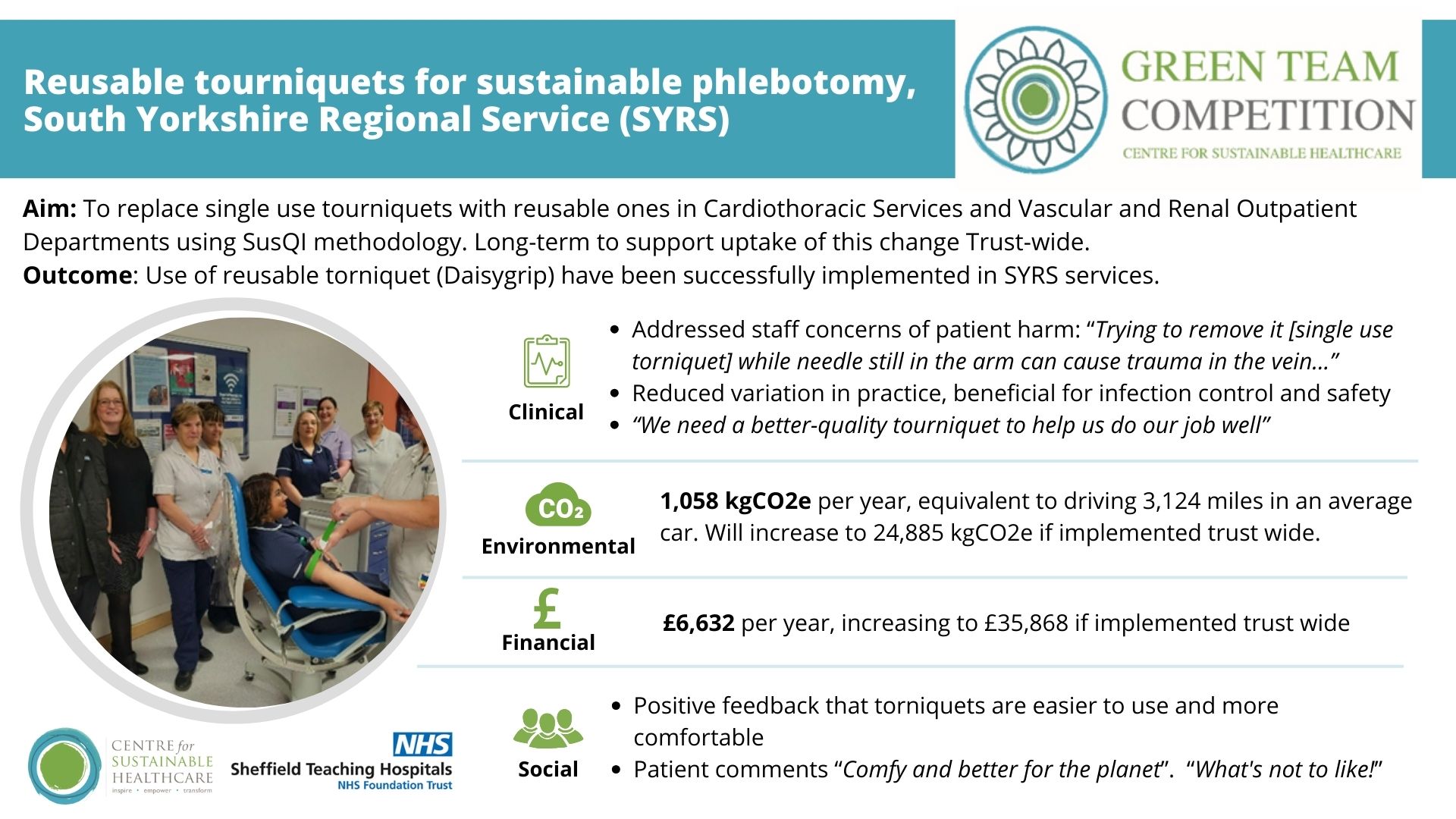
 Congratulations to the winning team, South Yorkshire Regional Services, for implementing reusable tourniquets for sustainable phlebotomy in their outpatient departments. The team have already taken steps to raise awareness and promote take up of this change across the Trust, with enthusiasm from other departments.
Congratulations to the winning team, South Yorkshire Regional Services, for implementing reusable tourniquets for sustainable phlebotomy in their outpatient departments. The team have already taken steps to raise awareness and promote take up of this change across the Trust, with enthusiasm from other departments.
Mark Tucket, Director of Strategy and Planning said “The SYRS project really spoke to the importance of good staff and patient engagement, and challenges the concept of single use not only for torniquets, but equipment generally across the Trust”.
The SYRS team was led by Rebecca Palmer, Nurse Lead for Governance Quality Improvement and Lea Lindley Senior Sister, Cardiology/Vascular Outpatients.
- Rebecca said “It has been absolutely inspiring to be a part of the competition. I’ve learned so much about the sustainable value equation and how to get the message across to our staff”.
- Lea said “Happy staff, happy patients – it’s a win-win all round!”
The Centre for Sustainable Healthcare would like to thank and congratulate all teams that took part in the competition. The competition's outcomes serve as proof of the teams' commitment and efforts to improving the sustainability of the healthcare system.
Green Team Competition Projects
Read the full Impact Report here or view the project summaries below.
- Reusable tourniquets for sustainable phlebotomy, South Yorkshire Regional Service (SYRS)
- Assessing the financial and environmental impact of sending phlebotomy trays for unnecessary external steam sterilisation, sexual health team
- A Greener Hospital Storeroom, Acute & Emergency medicine care group
- Rationalising drugs in the operating theatre, Operating Services, Critical Care and Anaesthesia (oscca) and Pharmacy
- Reducing Paracetamol Co-Prescribing with Strong Opioids on the Sheffield Macmillan Unit for Palliative Care, Palliative Care
- Extending the life of anaesthetic circuit tubing and rationalising our suction waste stream, Anaesthetics, Obstetric and Gynaecology Theatres
1. Reusable tourniquets for sustainable phlebotomy, South Yorkshire Regional Service (SYRS)
Team members: Rebecca Palmer Nurse Lead for Governance Quality Improvement; Lea Lindley Senior Sister, Cardiology/Vascular Outpatients; Tony Ward Senior Charge Nurse, Renal Outpatients; Nina Coggins Sister, Cardiology/Vascular Outpatients; Joanne Vaines Clinical Support Worker, Key phlebotomy Trainer; Steve Newsome Logistics Manager, SYRS; Paul Cattell Senior Charge Nurse Cardiac Catheter Suite
Setting / patent group: Phlebotomy testing for Cardiology, Cardiac Surgery, Thoracic Surgery, Vascular and Renal services
Issue: The single-use tourniquets used by SYRS were poor quality and provided a poor experience for both patients and staff. The high volume of torniquet required also contributed a lot of clinical waste.
Intervention: A reusable torniquet (Daisygrip) was trailed and has been implemented across the SRYS service via implementation of a communication and education strategy.
Outcomes
Within their trial of SYRS, the team has projected annual savings of £6,632 and 1,057 kgCO2e, equivalent to driving 3,123.7 miles in an average car. They will monitor their procurement data to confirm in one year if their estimated savings are correct or under/overestimated.
The team plan to promote the scale of this change Trust wide. Based on procurement data of single use items, this change could bring savings of £35,868 and 24,885 kgCO2e, equivalent to driving 73,493.7 miles in an average car.
Staff commented that they had concerns the single use torniquet could harm patients and agreed they wanted a better option, e.g.
- “Removing it [single use torniquet] is difficult and causes further discomfort as we wrestle with it. And trying to remove it while the needle is still in the arm and the last bottle being drawn can cause trauma in the vein while you're wrestling with it.”
- “We need a better-quality tourniquet to help us do our job well. Preserving our patients' veins is really important for their future as renal patients. Poor quality of single use can make patient experience stressful and poor. I feel this when I’m trying to take their blood”.
Following the trial, there was agreement the reusable torniquet is a better option for patients and staff. 94% staff said it was important to them that the reusable tourniquet would help to reduce waste and carbon emissions in the department. 100% of patients surveyed agreed they liked the reusable option, reporting it does not pinch or mark their skin or cause any pain.
Key learning point
The key elements that contributed to the success and learning of this project were the importance of keeping the weekly meetings going over the next 10 weeks. The team was extremely focused when it came to driving actions and tracking key milestones and risks. They learnt when things didn't go so well. Particularly around education, communication, and stock ordering. This helped them focus on our priorities, which were patient and staff engagement and listening to what mattered to them. They learned that staff education, product distribution, and stock control are important and need to continue beyond the project timeline. Involving the right people from the start and inviting colleagues in response to any issues that arise. With the support of the nurse director, operations directors, and the infection prevention and control team, they were able to make these changes happen.
Team members: Rachel Darling, Health Adviser
Setting / patent group: Sexual Health Outpatient Clinics
Issue: The sexual health team use blue phlebotomy trays to temporarily store components required to collect patient samples and to place treatments prior to administration. These trays have historically been sent for weekly steam sterilisation. The rationale for this was unclear.
Intervention: To stop unnecessary sterilisation of phlebotomy trays in the sexual health unit, by implementing a change to department policy. The team reviewed their current practice and confirmed with Infection Control that there was no barrier to stopping this process in favour of cleaning in the clinic.
Outcomes
Previously there were delays to patient care as staff members had to unpackage newly received blue trays to undertake sampling. Trays are now cleaned with tristel and cloth which were already available within each clinic room and are ready for use at the start of each clinic session. 13 trays are sent for sterilisation per week, equating to 21.48 kgCO2e. Projected across a year, this is a saving of 676 trays sent and 1,116.75 kgCO2e. This is equivalent to driving 3,298 miles in an average car.
Ending this cleaning will prolong the lifespan of the trays which have been warped and damaged from the sterilisation process, which may lead to additional savings. The change has been cost neutral as the department already pays a minimum charge for sterilisation requirements.
15 staff members completed the staff survey from 36 eligible clinicians ranging from Support Workers to Consultants.
- 80% of these team members were agreeable to stopping sending trays for external sterilisation.
- As the response was not unanimous, the team has explained to staff that it has been agreed by infection control that they do not require steam sterilisation and that they were available to discuss this further should anyone have any concerns.
- 73% of team members responded that they were very concerned about waste and the environmental impact of care. 6% were sometimes concerned while 20% had never considered it.
Key learning point
This is a very simple change of practice, challenging an unnecessary process that continued only because it was seen as "routine." Although a small project, it can hopefully be the start of positive change in the clinic. This change required staff engagement and has brought a real boost to morale within the clinic. Multiple staff members approached the team, acknowledging how they were moving forward with common-sense sustainability plans in the clinic. There is a passion at SHS for continuing to question their practices and develop them, and the team has been approached with further areas for improvement.
3. A Greener Hospital Storeroom, Acute & Emergency medicine care group
Team members: Dr Caroline Kendrick (Emergency Medicine Consultant); Dr Amy Fantham (Emergency Medicine Junior Clinical Fellow); Mr Gary Green (Storeroom Manager); Ms Amy Page (Deputy Operations Director)
Setting / patient group: Emergency department stockroom/medical supplies
Issue: The emergency department stockroom was poorly organised and not stocked appropriately, leading to frustration for staff and delays / issues in identifying items needed for clinical care.
Intervention: A comprehensive storeroom review with MDT involvement across clinical and non-clinical teams. Several meetings were arranged to review every product within the stockroom to determine whether items were still in use within the department, if appropriate amounts were being ordered and how decisions were made regarding when and what to reorder.
Outcomes
During the 10-week project approximately 25% of the storeroom was reviewed. Changes made amount to projected annual savings of £20,786 and 10,810 kgCO2e, equivalent to driving 28,539 miles. The team plans to review the remaining 75% of the stock room so there is potential to significantly increase these savings.
Staff commented they think often about the waste generated in emergency, and that working in an environmentally friendly department is important to them. Before starting the project, staff feedback was largely that the storeroom was cluttered, intimidating and made it challenging to find items needed. The team anticipates a more organised storeroom and inventory control system will help facilitate saving staff time and improving the overall user experience. They will re-survey staff on completion of the project.
Key learning point
As a group the team was overwhelmed by the amount of stock present and soon realised the enormity of the task ahead. However, pulling together they became enthused by the changing landscape of the room and results being achieved. The project has also provided a springboard for many other sustainability project ideas within the department.
The main message to take away from this project is that if you start with a small snowflake, you could end up making a snowman!
Team members: Tim Orr (Consultant Anaesthetist); Caroline Dalton (Recovery Lead Practitioner); Matt Clarke (Principal Pharmacist, Medicines Information)
Setting / patent group: Theatres
Issue: Medication storage in theatres.
Although generally very safe, anaesthesia is a specialty with a high risk of adverse events which need to be managed rapidly to prevent patient harm. For this reason, many medications are immediately available in case their use becomes necessary. Good medicines handling practice prohibits the splitting of boxes to individual ampoules/doses and so whole boxes of medications that are rarely used are stocked in multiple areas in case their use becomes necessary and sometimes to accommodate clinician preference. Many of these boxes expire unopened and require disposal and replacement.
There is a limited storage space for medications in operating theatres, the visual appearance of products may change from week to week due to manufacturer preferences or supply chain problems necessitating alternative sourcing arrangements and different medications often look similar. The risk of medication errors in this setting is high with significant potential harm to patients and there are multiple examples in the literature and locally of this3. In addition to patient harm, the impact of medication errors on the staff involved is significant and also harmful.
Intervention: Reducing the medication burden in theatres whilst maintaining adequate availability of emergency medications has the potential to bring safety, financial, social and environmental benefits. The team reviewed all medications in the anaesthetic rooms in their operating theatres to identify which medications were not used, could be ordered less (low use drugs) and moved to a centralised location.
Outcomes
Any reduction in the number of medications stocked within anaesthetic rooms and theatres, whilst maintaining an accessible central supply, reduces the chaos and variation in the drug cupboards. This reduces the risk of medication error with consequent benefits to patient safety provided rapid and reliable access is maintained for relevant emergency medications.
As part of the audit, several examples of poor drug management practices such as local anaesthetics stored with other drugs and expired drugs were identified and rectified. Feedback to the relevant staff groups provided an opportunity to improve medicines management with a consequent reduction in risk to patient safety.
The modelled carbon saving for 12 elective theatres and 3 obstetric is £11,300 and 7,017 kgCO2e, equivalent to driving 20,723 miles in an average car.
A survey was sent to all obstetric anaesthesia consultants:
- 11/14 responded (79%)
- 10/11 (91%) were supportive of the principle of centralising low-use medications
- 9/11 (82%) had no concerns about the proposal. 2/11 (18%) were concerned it could delay emergency treatment or that they would “forget where they are”
- 10/11 respondents could see benefits in centralising stock and thought there were sustainability savings, 8/11 (73%) cost savings and 7/11 (64%) reduction in risk from simplifying the cupboards.
The team also sent a survey to their pharmacy technician who strongly thought this intervention would make their job easier, save them time, save money and reduce wastage
Key learning point
MDT / cross-departmental communication and aligning the aims with wider organisational goals has been key to this project. Centralising low-use drugs within our operating complexes is achievable, clinically acceptable and will result in financial savings as well as environmental, workplace and potentially safety improvements. The team has consulted with governance, pharmacy and anaesthetic colleagues to develop a process to implement this change across the trust which will bring larger savings.
Team members: Dr Kay Stewart Consultant in Palliative Medicine; Dr Hayley Evans SpR in Palliative Medicine; Miss Fiona Stephenson, Clinical Pharmacist
Setting / patent group: Macmillan Unit for Palliative Care (MPCU) - an 18-bedded NHS funded palliative care in-patient unit.
Issue: Patients have historically been prescribed regular paracetamol, despite evidence supporting that paracetamol is not effective for patients who are already taking strong opioids for pain management. Clinicians are often reluctant to stop paracetamol “in case it makes things worse” but will do so, usually with no change in symptom control, when the patient begins to struggle with their medication burden. Prescription and administration of low value drugs leads to unnecessary medicines use and waste
Intervention: The team aimed to review medications prescribed on admission to MPCU (already part of the admission process) and consider, jointly with the patient, whether moving paracetamol to the “as required” part of the medication prescription would reduce the medication burden to the patient, with no change to pain control, reduce nursing time spent administering an ineffective treatment and reduce waste (time, money and physical waste) on the ward.
They ran short education sessions with the nursing and medical team. The team aslo produced a poster to put up in clinical areas showing the waste associated with paracetamol administration along with some measurements of time spent/cost to encourage the prescribers and administrators of paracetamol. They initially hoped for a 50% reduction in the usage of paracetamol on MPCU.
Outcomes
This project ran for 10 weeks, interrupted by industrial action and a covid outbreak on the ward. A snapshot of the patient medications prescribed before the project revealed (10/18, 55%) were prescribed regular paracetamol. By the end of the study period, an average of 3.5/18 (19%) patients had regular paracetamol prescribed, a 36% reduction in regular paracetamol usage.
Of the 19 patients that had switched to prn paracetamol on admission, only six doses of paracetamol were administered in a two week period. If the patients had stayed on regular paracetamol on admission to MPCU, each patient could have had 56 doses in 2 weeks, a total of 1,058 doses avoided. No patient that was switched to prn paracetamol had a regular dose reinstated during the project period.
A 36% reduction will bring an annual saving of £211.2 and153.88 kgCO2e, equivalent to 454 miles driven in an average car, or a return trip between Cardiff and Leeds. The project has also saved staff time and will save stock space on the unit.
Staff were receptive to the project change. Many had not realised the cumulative time impact of relatively “simple” analgesia but were not surprised when presented with data to show time taken to administer. It was found that paracetamol was often the medication omitted as not being seen as important when patients started to struggle to take their medications. The project therefore has potential to reduce tablet burden to patients.
Key learning point
The project nudged the team to make a small change with a relatively big impact which would positively benefit the patients (reduced medication burden compared to perceived effect), the nursing staff (time saved administering paracetamol), the environment (kgCO2 saved), the drug budget (money not spent) with little impact on the medical staff enabling the change (asking if the patient felt the paracetamol helped and would they like to not have it regularly if not).
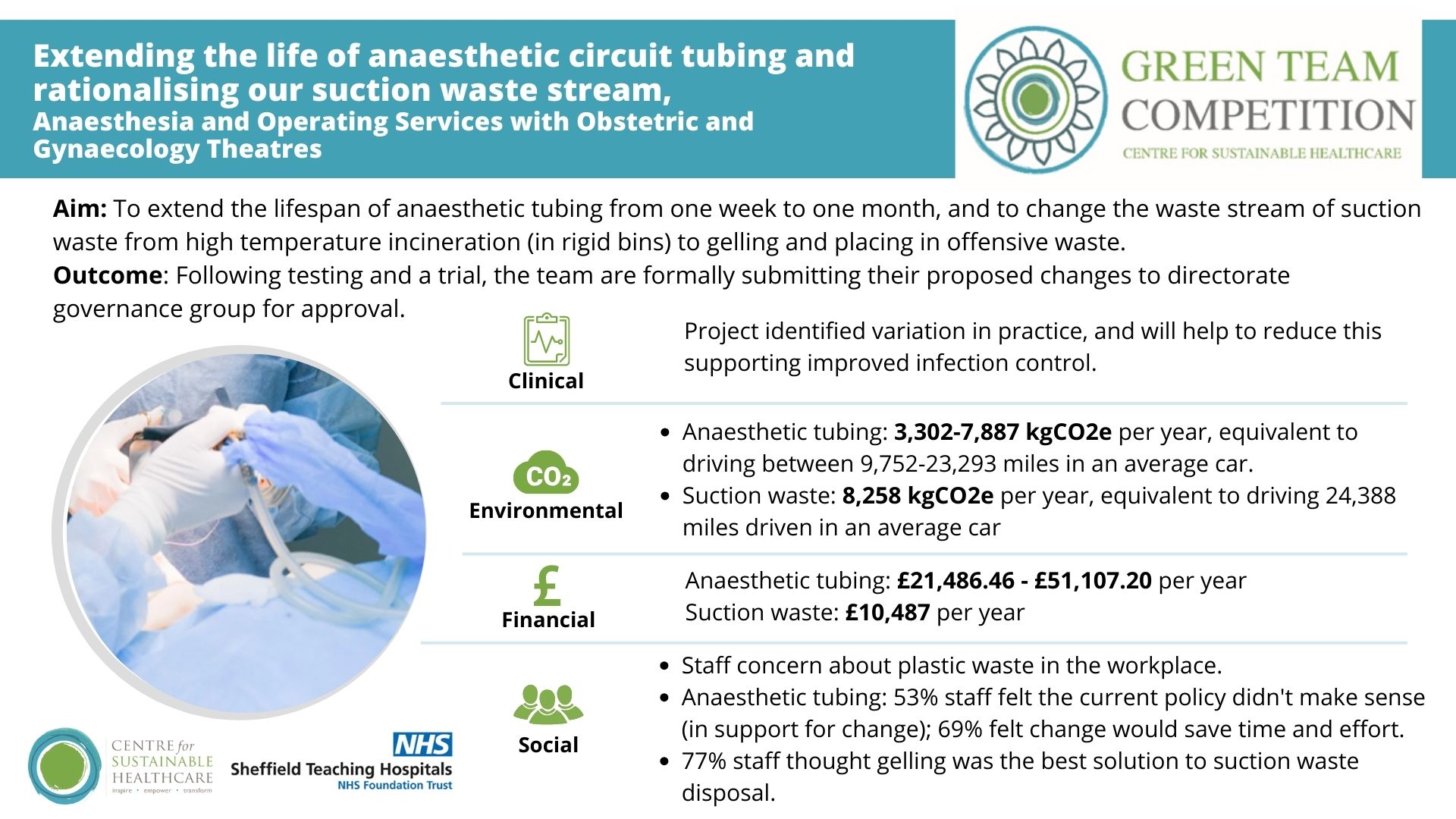
Team members: Tim Orr, Consultant Anaesthetist, Sustainability Lead Anaesthesia and Operating Services; Poppy Robinson, Senior Operating Department Practitioner, Obstetric and Gynaecology Theatres
Setting / patent group: Obstetric and Gynaecology Theatres
Issues:
- Plastic breathing tubing is routinely used to connect patients to anaesthetic machines for ventilation and oxygenation enabling surgery under general anaesthesia. It may also be used to deliver nitrous oxide analgesia in the operating theatre. Breathing tubing for anaesthetic machines is validated by the manufacturers for 7 days use. This is an arbitrary duration and lacks scientific basis. The product does not need to be sterile, is not intended to be single patient use and the bacterial/viral filter is trusted to prevent respiratory pathogens contaminating the circuit and causing transmission of hospital acquired respiratory infections
- Suction waste in the operating theatre is collected in plastic bags which should not be disposed of in the offensive waste stream because they are liquid and risk leakage. In the past, gelling agent was used to solidify the waste. In 2020, the National Patient Safety Agency issued an alert, restricting the use of gelling agent to “exceptional use only via a specialist team”. This led to the indiscriminate removal across our trust and suction waste in our maternity unit is now disposed of by high temperature incineration as anatomical waste in a rigid single-use bin.
Interventions:
- Circuit tubing: To extend the lifespan of the tubing from one week to one month (a 75% reduction). The team identified widespread confusion and variation in practice relating to changing different components of the circuit and a misunderstanding of the infection control implications. They estimated a worst case number of uses over a period of a month and trialled robustness. They gained directorate governance group and infection prevention and control approval to introduce the change at Jessops (three theatres) for a period of 3 months as a pilot. If successful, the team will then roll out across all the theatres.
- Suction waste: The team estimated current carbon footprint of disposing of their suction waste in the current stream and model the use of gelling agent and disposal in the offensive waste stream.
Outcomes
Circuit tubing: their modelled figures differed from procurement data, so they have estimated a range in potential annual savings from £6,416-£51,107. They would save between 3,302-7,887 kgCO2e, equivalent to driving between 9,752-23,293 miles in an average car. However, the team should be working to a standard practice and if they were to move towards this, the higher figure would be representative.
There was widespread acknowledgement that the proposed intervention would reduce plastic waste and save money:
- 9/13 (69%) thought it would save them time and effort
- 7/13 (53%) thought the current policy, as they understood it, didn’t make sense, demonstrating approval for our proposed changes
Suction waste: Converting to gelling and disposing their suction waste in the offensive wastestream across maternity theatres would result in £10,487 and 8,258 kgCO2e saved, equivalent to driving 24,388 miles driven.
- 10/13 (77%) thought gelling and disposal in a bag was the best solution to suction waste disposal in Jessops
- 5/13 (38%) of respondents thought gelling waste instead of boxing it would reduce their workload, the remainder thought it would have a neutral effect
- Nobody thought it would add to their workload
Key learning point
Staff engagement has been key to this project. It has been quite easy to gain acceptance in principle and highlights the tendency to make changes that have a destructive effect on the environment and costs without considering the consequences and alternatives.