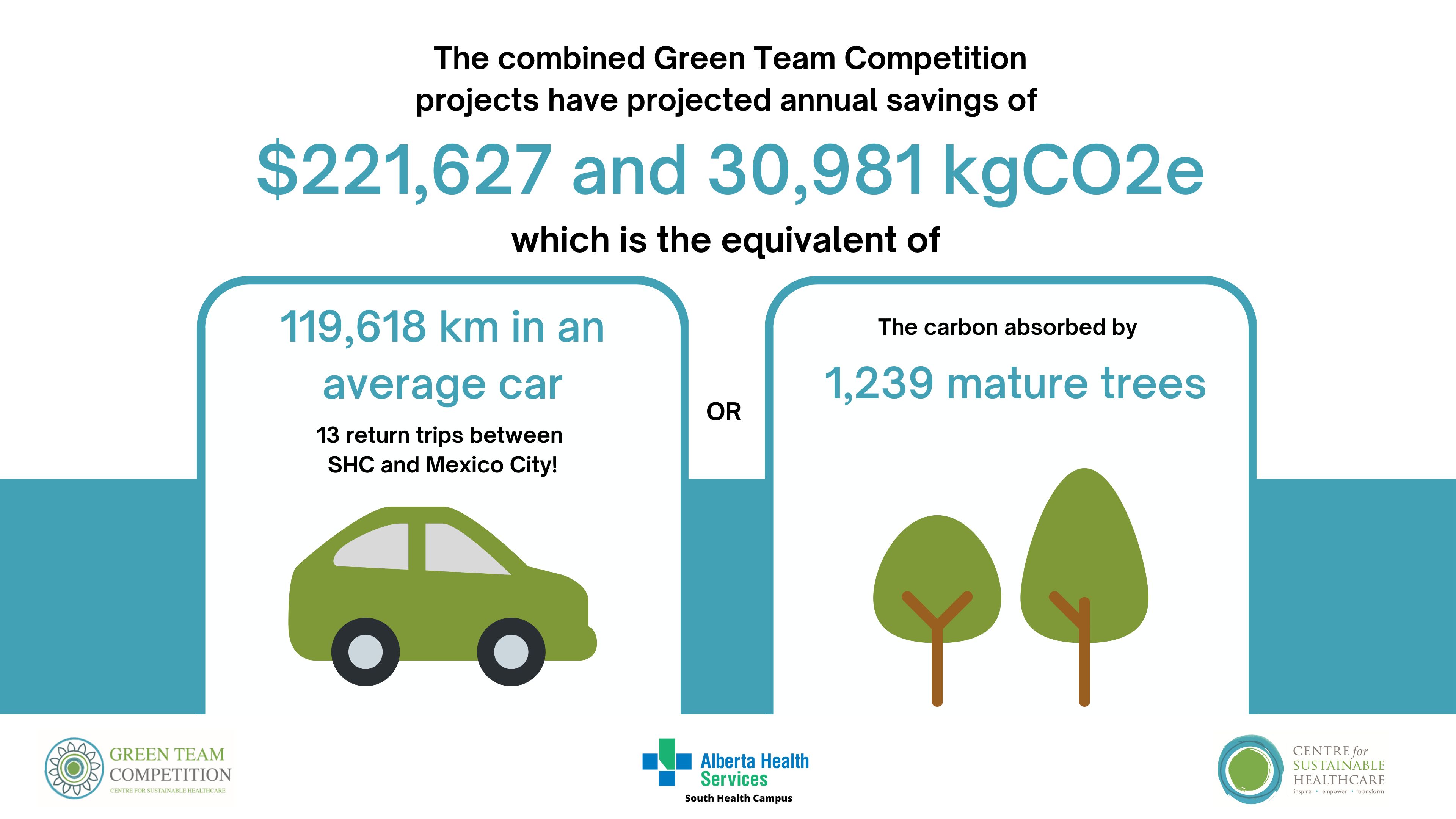
South Health Campus, Alberta Health Services Green Team Competition expected to save $221,627 and 30,981 kgCO2e annually
In May of this year, South Health Campus (SHC), one of the four adult care centres in the Calgary Zone, Alberta Health Services, Canada, commenced a Green Team Competition in partnership with the Centre for Sustainable Healthcare. The competition has brought anticipated annual savings to the hospital of $221,627 and 30,981 kgCO2e. This is the carbon footprint equivalent of driving 119,618 km in an average car (or 13 return trips between SHC in Alberta and Mexico City!).
SHC embarked on a journey to embed sustainability into quality improvement, recognising healthcare’s impact on greenhouse gas emissions, with improving patient outcomes and providing value-based care being the key motivations underpinning this work. Over the past year, SHC has become the first North American internationally recognised Beacon site and run the first international Green Team Competition. This created awareness, stewardship, and a buzz around environmental sustainability in everyday practice.
Through the Green Team Competition, six teams from SHC were selected to engage in our award-winning programme in sustainability in quality improvement (SusQI) that transforms expert knowledge into action. Each team received mentoring from CSH facilitators to drive healthcare transformation by developing, implementing, and measuring the impact of projects through the lens of the sustainable value equation.
 At the 19th September presentations, the teams showcased their projects, including the anticipated savings and future opportunities, to an audience of key stakeholders in the SHC sustainability journey, their fellow teams, and the judging panel, which included:
At the 19th September presentations, the teams showcased their projects, including the anticipated savings and future opportunities, to an audience of key stakeholders in the SHC sustainability journey, their fellow teams, and the judging panel, which included:
- Sean Chilton, Interim Vice President and Chief Operating Officer, Clinical Operations and EMS, AHS
- Dr Colin Del Castilho, Site Medical Director, South Health Campus
- Harry Vandermeer, Executive Director, Office of Sustainability & Energy Management, AHS
- Patty Wickson, Executive Director, Innovation, Evidence, Evaluation & Impact, AHS
- Dr Frances Mortimer, Medical Director, Centre for Sustainable Healthcare (CSH)
The winning and highly commended teams (announced below) have been invited to present at an SHC-wide Green Team Competition and Quality Improvement Showcase event during the week of 21st - 25th October 2024 to share their impressive impact widely. All teams will have their work displayed through poster presentations.
"It was truly a privilege to participate as a member of the judging panel in the sustainability competition at South Health Campus in Calgary. I was quite amazed not only of the number of participants, but also the quality of the presentations and the number of people that made up the six teams, particularly at a time when healthcare systems not only in Calgary but across Canada are feeling so stressed. The creativity put into the various projects and the excitement and passion of the presenters to not only see the impact of their project in their department, but also the vision they had of how the project could be expanded to other departments at South Health Campus and to other facilities across Alberta was insightful. Every presentation was first class."
Harry Vandermeer, P. Eng., Executive Director, Office of Sustainability & Energy Management
 WINNERS: Emergency Department
WINNERS: Emergency Department
Congratulations to the winning team, the Emergency Department, led by Cassandra Carrier, Quality Improvement Lead RN, and Daniela Moreira, Emergency Department Unit Manager.
The Emergency Department team successfully reduced the amount of equipment required during the administration of IV ketorolac (a pain relief medication)—a change that was welcomed by pharmacy and nursing staff, with the potential to provide pain relief to patients sooner. There is scope and ambition at SHC to expand the initiative to other medications and to other settings.
"The green team competition successfully built the foundational skills such as carbon emissions calculation which can be further incorporated into future quality improvement project. Sustainability in healthcare is now at the forefront our quality improvement mindset. The experience was truly eye opening.”
Emergency Department Team
HIGHLY COMMENDED: Outpatient Neurology
Congratulations to the highly commended team, the Outpatient Neurology team, led by Megan Yaraskavitch, Physician Lead, General Neurology Program and Neurology Central Access and Triage, Quality Improvement Lead, Division of Neurology, and Vikram Karnik, Site Lead, Clinical Neurosciences, South Health Campus, and Director, Adult Neurology Residency Program.
The team have optimised their use of virtual consultations to bring social and financial benefits to patients. A key driver of the project’s success was the motivation of the physician group to do “something” to make healthcare more sustainable. The team hopes that by starting small, they can measure the impact more easily, creating a case to expand to other areas within their department.
“Prior to this competition, I was unaware of the significant impact our healthcare system has on environmental sustainability. Presenting this impact to our group, provided a sense of “urgency” to change how we are delivering care. Engagement was increased as a result. I am hopeful that with this messaging, there will be ongoing motivation to continue to scale and spread our learnings. Thank you for this opportunity.”
Megan Yaraskavich, Neurology Team
The Centre for Sustainable Healthcare would like to thank and congratulate all teams that took part in the competition. The competition's outcomes serve as proof of the teams' commitment and efforts to improve the sustainability of our healthcare systems.
Green Team Competition Projects
Read the full Impact Report here or view the project summaries below.
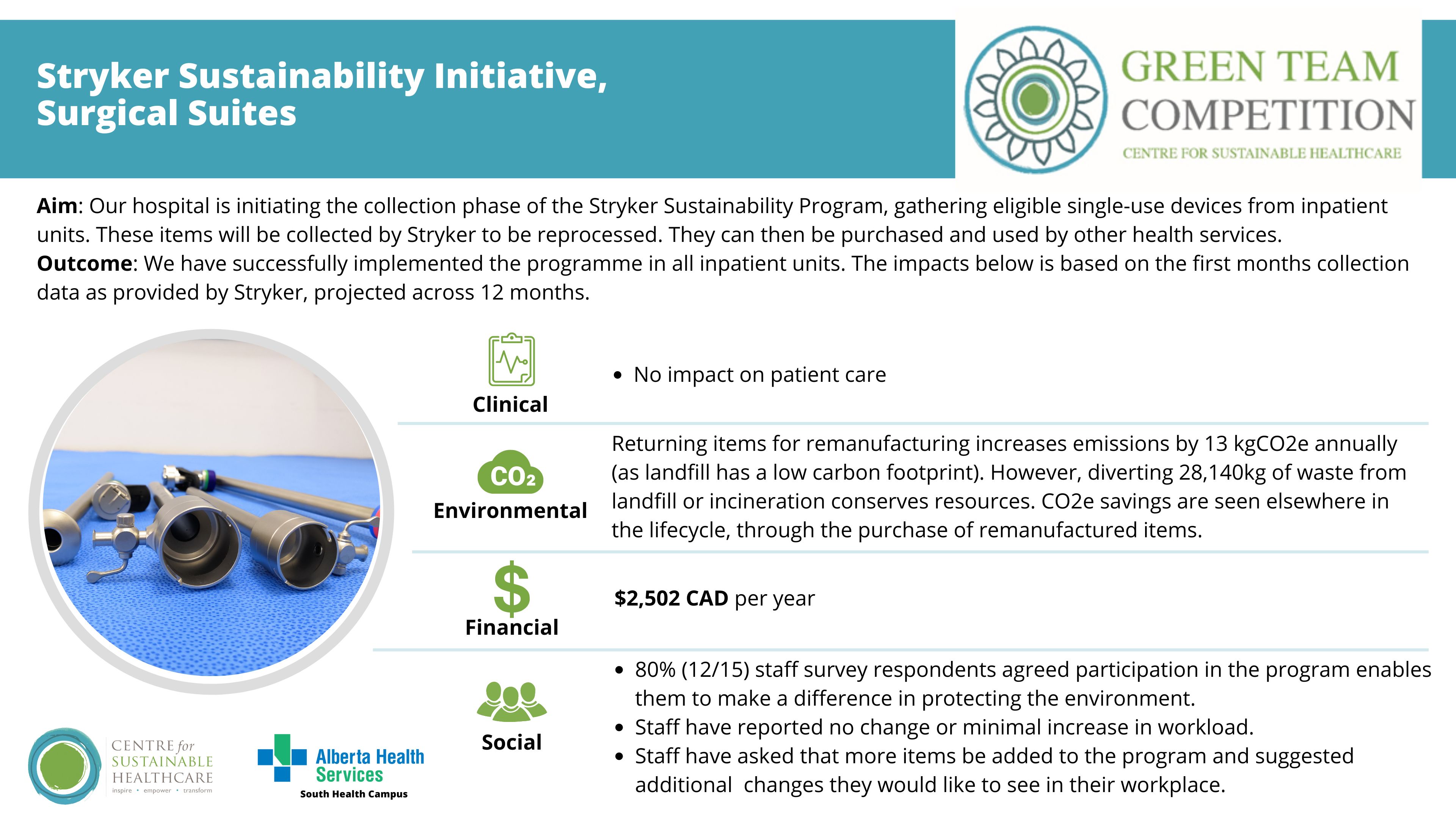
Team members: Michelle Shand (Program Manager - Surgical Services); Rachel Taylor (Program Manager - ICU/CCU, Respiratory Services, Pulmonary Diagnostics and Bronchoscopy Suite); Ermin Sabic (Environmental Services Manager); Mark Drescher (Site Services Supervisor - CPSM Support Services); Simon Robinson (Clinical Nurse Educator - Surgical Suites & Minor Surgery Clinic); Jelena Poprzen (Clinical Quality Improvement Consultant); Pedro Reis (Surgery Sustainability Lead)
Setting / patient group: Inpatient units, operating theatres, and the Emergency Department
Issue
Single-use medical equipment contributes significantly to costs and carbon emissions, right from procurement to waste disposal. These types of items are used in all areas of acute care and in the operating rooms. At SHC alone, the team sends over 5,000 single-use compression stockings to the landfill every year. Within Calgary, three adult sites have implemented the Sustainability Solutions Program through Stryker. The goal at SHC is to join this initiative to be in alignment with their partner sites and to better support the planet.
The Stryker Medical Equipment Remanufacturing Program, known as the Sustainability Solutions Program, focuses on the collection and reprocessing of medical devices to reduce waste, extend item lifecycles, and lower healthcare costs. For organisations that send back repurposed devices, savings can be made in waste disposal costs and carbon emissions. For organisations that buy remanufactured items, they save money and reduce carbon emissions related to the manufacturing and procurement of devices.
Intervention
Inpatient units, operating theatres, and the Emergency Department were asked to participate. Those that had the capacity to join this initiative were oriented to the programme.
The Stryker recycling programme was initially launched at Rockyview General Hospital (RGH), and the team at South Health Campus (SHC) adapted it to fit their site-specific needs. After meeting with RGH’s site champion and Stryker representatives, the team at SHC collaborated with the supply manager and environmental services to develop a collection process. Unit champions were identified, and hampers and bins were distributed, with a collection schedule set for every two weeks. Educational materials were provided to staff. All materials were supplied by Stryker at no cost, and since the programme's launch in May 2024, additional units have expressed interest in joining.
Outcomes
Patient outcomes: No impact on patient care.
Environmental sustainability: Sending items back to Stryker creates a small increase of 13.17 kgCO2e per year. However, the project will result in 28,140 kg of waste being diverted annually from landfill or incineration. Diverting waste from landfill or incineration is environmentally beneficial because it conserves natural resources and supports the reuse and recycling of materials, contributing to a more sustainable product life cycle.
While this results in a minor increase in emissions for SHC, savings will be reflected in the purchasing of remanufactured items from other hospitals, which could not happen without the team at SHC, AHS, and others engaging in the return scheme. Based on the volume of items they are returning, they will save 3,431 kgCO2e.
Economic sustainability: The projected annual savings from diversion from waste streams (general landfill waste and incineration) are $2,502 CAD, based on the first month’s waste diversion data provided by Stryker. These savings will increase as additional units join the initiative.
Social sustainability: Preliminary staff survey results after two weeks indicated that the programme has been positively received, with no change or minimal increase in workload (which was expected due to the nature of the change). 80% of respondents agreed that participation in the programme enables them to make a difference in protecting the environment. Staff have asked that more items be added to the programme and suggested additional environmentally focused changes they would like to see in their workplace.
Key learning points
The main driver for the success of the programme is staff motivation to do their part and make sustainable choices in the workplace. The programme also sparked an interest in suggesting further sustainability ideas. Comments in the survey indicated that there is an appetite among staff to include more items in the recycling programme. Further increasing staff awareness of the impact that healthcare delivery has on the environment and providing opportunities for staff to “do something” about it is the first step in creating more sustainable processes.
2. The Sustainable Value of Culinary Medicine and Teaching Kitchen Programs: Expanding the South Health Campus Wellness Kitchen Operational Model to a Satellite Teaching Kitchen to Support Cancer Patient’s Access to Care within AHS
Team members: Julia MacLaren (Wellness Kitchen Consultant, South Health Campus); April Matsuno (Wellness Centre Manager, South Health Campus)
Setting / patient group: Oncology patients
Issue
Cancer patients often face challenges in maintaining proper nutrition, which is critical for improving treatment outcomes and quality of life. Culinary Medicine (CM) and Teaching Kitchens (TK) offer a practical, evidence-based approach to helping patients and caregivers develop food preparation skills aligned with their dietary needs. However, these programmes are underutilised in Alberta's oncology care system.
Intervention
The SHC Wellness Kitchen, the first Teaching Kitchen (TK) in Alberta, provides Culinary Medicine (CM) programmes that combine practical cooking lessons with evidence-based nutrition guidance. This initiative, launched in collaboration with clinical teams and community organisations, aims to improve the health outcomes of cancer patients by addressing nutrition challenges during treatment and recovery. The Wellness Kitchen team proposes expanding this model to a satellite TK at an AHS Cancer Centre, integrating CM into oncology care pathways. This model promotes prevention, self-care, lean clinical pathways, and low-carbon alternatives. Improving patient nutrition has the potential to reduce the intensity of oncology interventions such as surgery, radiation, and medication, and optimise outcomes for patients.
Potential Impacts
Clinical Sustainability: CM interventions improve cancer patients’ nutritional status, which supports healing, reduces treatment side effects, and enhances tolerance to therapies. The programme promotes better surgical outcomes, reduces hospital stays, and helps decrease overall cancer morbidity and mortality. Integrating CM into cancer care pathways also boosts clinician awareness and increases referral rates, enhancing patient access to these valuable resources.
Environmental Sustainability: The CM programme’s potential to reduce intensive treatments such as surgery, chemotherapy, and hospital stays translates into significant carbon savings. For example, improving nutrition to reduce nausea during chemotherapy could eliminate the need for antiemetic medicines. If just one dose of Olanzapine was prevented in 1,000 patients, CO2e emissions would be reduced by over 13,569 kgCO2e—equivalent to driving from Calgary to Fredericton. Virtual CM classes further reduce emissions by decreasing the need for patient travel.
Social Sustainability: CM programmes foster a sense of community and reduce feelings of isolation for cancer patients and their caregivers. By offering virtual sessions, the initiative provides more equitable access to care for rural patients and those facing mobility or logistical challenges. Caregivers gain confidence in managing patients’ nutritional needs, improving both patient and family well-being.
Financial Sustainability: The long-term financial savings of CM programmes are substantial. Reduced need for medications, shorter hospital stays, and fewer complications lead to lower healthcare costs. For instance, reducing Olanzapine use by one dose each in 1,000 patients could save $18,790 CAD. Additionally, the efficient use of TK spaces and virtual programming minimises operational costs while expanding patient reach.
Key learning point
Leveraging the operational efficiencies, skill set, experience, and expertise of the SHC Wellness Kitchen and its team, a satellite model of operations to establish a CM strategy in cancer care has significant potential to improve clinical integration, provide timely patient access to oncology-specific CM care, and enhance experiences and outcomes for cancer care patients and their caregivers. The satellite model aligns with the Centre for Sustainable Healthcare principles of sustainable practice, offering opportunities for prevention, patient empowerment and self-care, lean clinical pathways, and low-carbon alternatives to improve all parameters of the triple bottom line (environmental, social, and financial impacts) of sustainability in cancer care in Alberta.
3. Minimising desflurane use and decreasing fresh gas flows, Anesthetics
Team members: Vivian Ip; Nathan Brown; Alan Chu; Leyla Baghirzada; Joanna Fifen; Esther Ho; Ryan Endersby
Setting / patient group: Anesthesia department
Issue
Not all anaesthetic volatile agents have the same environmental impact. Evidence from life cycle analysis has shown that desflurane is significantly more carbon-intensive compared to sevoflurane, with a global warming potential (GWP) 2,540 times that of carbon dioxide for desflurane versus 130 times for sevoflurane over 100 years. Furthermore, desflurane is less potent, which means more than three times as much agent mass is required to produce the same clinical effects. Recent literature has also demonstrated that occupational exposure to desflurane poses a potential health hazard to healthcare personnel, with associated genetic damage and oxidative stress. A recent quality improvement project showed that reducing the use of desflurane resulted in a 58% reduction in associated costs.
Intervention
To implement changes, an email was sent to all anaesthesiologists at South Health Campus to gather feedback, identifying six desflurane users who were then approached individually. Initial resistance led to a stepwise approach, starting with a lecture on environmental sustainability, followed by placing stickers on anaesthetic machines highlighting gas emissions. Desflurane vaporisers were relocated to increase inconvenience, and reminders to use low fresh gas flow and end-tidal control were placed on machines and charting computers. Data on desflurane and sevoflurane usage, as well as anaesthetic cases, will be collected three months before and after the changes to assess impact.
Outcomes
Patient Outcomes:
- Clinically, there is no risk in switching from desflurane to sevoflurane or using low fresh gas flow. In fact, there are more risks of adverse effects associated with using desflurane than sevoflurane. For instance, desflurane is an irritant and may cause bronchospasm, increase sympathetic response, increase cerebral blood flow, and raise cerebrospinal fluid pressure, which can be detrimental in certain situations. As desflurane has reduced potency, a higher quantity is required to produce the same clinical response compared to sevoflurane.
- There is a small perceived benefit of earlier wake-up times with desflurane compared to sevoflurane; however, the undesirable effects outweigh the purported benefit of earlier recovery. With a better understanding of the pharmacokinetic properties of sevoflurane, anaesthesiologists can learn to adjust the dosage of sevoflurane towards the end of surgery and equalise the recovery times between desflurane and sevoflurane.
Environmental and Economic Sustainability: Following the changes, and accounting for the increased case volume in 2024, a 17% reduction in desflurane usage and a 6% increase in sevoflurane usage were observed when compared to the average monthly usage in 2023. This translates to a saving of 12 tonnes of CO2e, equivalent to driving 46,332 km in an average car. The team is currently working on retrieving financial data to produce meaningful and accurate financial results.
Social Sustainability: Two staff members raised concerns about relocating desflurane to the supply room due to potential impacts on professional autonomy. A stepwise approach was adopted to help them gradually adjust and understand the benefits of low fresh gas flow, end-tidal control, and the adverse effects of desflurane. Differences in the pharmacokinetics of desflurane and sevoflurane were highlighted, along with updated CAS guidelines and the growing focus on environmentally sustainable anaesthesia in other Canadian provinces, underscoring the broader health benefits of these changes.
Key learning point
This project has been extremely valuable for team bonding, educating other anaesthetists, and recognising the importance of social aspects when implementing changes. The key elements that contributed to the success and learning in this project include the need to assess the department’s or team’s emotions regarding changes and then implement those changes in a stepwise approach after thorough discussion.
4. Thinking Outside the Bag: Ketorolac IV Direct Administration at South Health Campus, Emergency Department
Team members: Cassandra Carrier, Quality Improvement Lead RN; Daniela Moreira, Emergency Department Unit Manager
Setting / patient group: Emergency department
Issue
Variations in IV administration can affect the consumables required, potentially increasing costs, carbon emissions, and time. One example is the use of mini-bags, where medication is diluted in 50-100 mL of IV fluid before infusion. This process can increase nursing workload, delay medication administration, and use more resources. In contrast, direct IV administration offers faster, more precise delivery, especially in emergency settings. To explore this, a project focusing on Ketorolac, the fourth most administered IV medication in the South Health Campus Emergency Department, was chosen due to the volume of orders and its minimal impact on pharmacy workflow.
Intervention
Stakeholders, including Pharmacy, the Contract, Procurement & Supply Management (CPSM), and clinical staff, were engaged. Pharmacy adjusted the Electronic Health Record (EHR) order setup to specify the correct administration route. This modification empowers nurses to decide how the medication should be administered. The Emergency Department nurses were involved in daily huddles, where the team shared relevant updates about the project's scope, goals, and potential benefits. The team collaborated with bedside nurses to obtain measurements for process analysis, such as the average time of medication preparation prior to implementation. To foster engagement, posters were designed for frontline staff, highlighting concrete information on expected financial, environmental, and social impacts. Educators and mentor nurses were identified early on as key resources to provide education, guidance, and support as needed.
Outcomes
Patient and Clinical Outcomes: Patients feel their needs are being met without excessive use of supplies and in a more timely manner. Obstacles to mobility and movement were also reduced. Administering ketorolac IV directly over 15 seconds may reduce the medication onset time by approximately 19 minutes, although the onset of pain relief was not specifically measured. The average physician assessment-to-discharge time was reduced by 6%, and the average medication order-to-administration time was reduced by 14% when comparing the one-month pre-implementation and post-implementation periods.
Environmental and Economic Sustainability: The projected annual savings in medical supplies amount to $23,266.56 CAD and 1,271.95 kgCO2e per year, equivalent to driving 4,911 km. These savings are attributed to reduced procurement (supply chain) and disposal of medical items, as well as reduced energy usage from pumps.
The procurement team reported a 25% reduction in mini-bag orders in the Emergency Department during the post-implementation period. Although site-wide ordering of mini-bags was not monitored, it is likely that a decrease in usage occurred in other departments due to the site-wide EHR change.
Social Sustainability: The elimination of an IV pole and pump was identified by patients as an improvement in their overall experience. Nurses indicated that they were comfortable administering ketorolac IV directly. The majority of nurses noted that the change in process positively impacted patient experience and decreased their workload.
Key learning point
A critical factor in our success was selecting a medication with straightforward administration, which garnered strong support from bedside nurses. Notably, we observed enhanced safety in medication administration—an unexpected improvement that we are eager to share with the pharmacy team. By disseminating these findings, we aim to raise awareness and facilitate the extension of this approach to other IV medications. The significant and broad ramifications that one change can have across multiple areas is both encouraging and inspiring.
5. Making Virtual Healthcare a Reality, Outpatient Neurology
Team members: Megan Yaraskavitch: Physician Lead, General Neurology Program and Neurology Central Access and Triage, Quality Improvement Lead, Division of Neurology, Clinical Associate Professor, University of Calgary; Vikram Karnik. Site lead, Clinical Neurosciences, South Health Campus, Director, Adult Neurology Residency Program, Clinical Assistant Professor, University of Calgary
Setting / patient group: General Neurology Clinic. Outpatient follow up appointments for patients with a diagnosis of “migraine”, “headache”, “other migraine”, and “epilepsy”.
Issue
Emissions caused by transportation to and from the clinic can be quite significant, especially in a city with relatively poor public transport and at a site that serves a large catchment area, often requiring patients to travel long distances to attend. Time spent travelling to and from appointments, as well as time spent in the waiting room, can often exceed the duration of the appointment itself. Appointment times are generally longer, meaning fewer patients can be seen, and at our centre, 7.4% of in-person follow-ups were not attended, whereas only 5.0% of virtual visits were “no shows”. In-person appointments also require additional nursing and clerical staff.
Intervention
The aim is to reduce the number of in-person follow-up appointments at the South Health Campus General Neurology Clinic by 30% over six months, leading to long-term ecological, social, and financial benefits for patients and the healthcare system.
Outcomes
The team extrapolated the potential benefits prior to implementation.
Patient Outcomes: A reduction in the no-show rate is anticipated, which may, in turn, improve patient outcomes and access to care.
Environmental Sustainability: It is estimated that replacing 30% of in-person visits with virtual appointments (352 appointments) would save 12,034 kgCO2e per year, equivalent to driving 46,463 km in an average car.
Economic Sustainability: The project incurred a one-time cost of $700 CAD for equipment. There is an inherent cost avoidance, as fee codes for virtual care are lower than those for in-person assessments.
Social Sustainability: Patients will save money on fuel, parking, and meal costs, and regain approximately one hour of time. Family members, who attended half of the appointments, would save similar amounts in terms of time and costs. Although staff have not been formally surveyed, there has been significant positive feedback towards this project during preliminary physician meetings, with several physicians keen to expand this initiative beyond the General Neurology Clinic.
Key learning point
A key driver of the project’s success was the motivation of the physician group to “do something” to make the healthcare system more sustainable. The hope is that by starting small, the impact can be measured more easily, creating a case for expansion to other areas within the department.
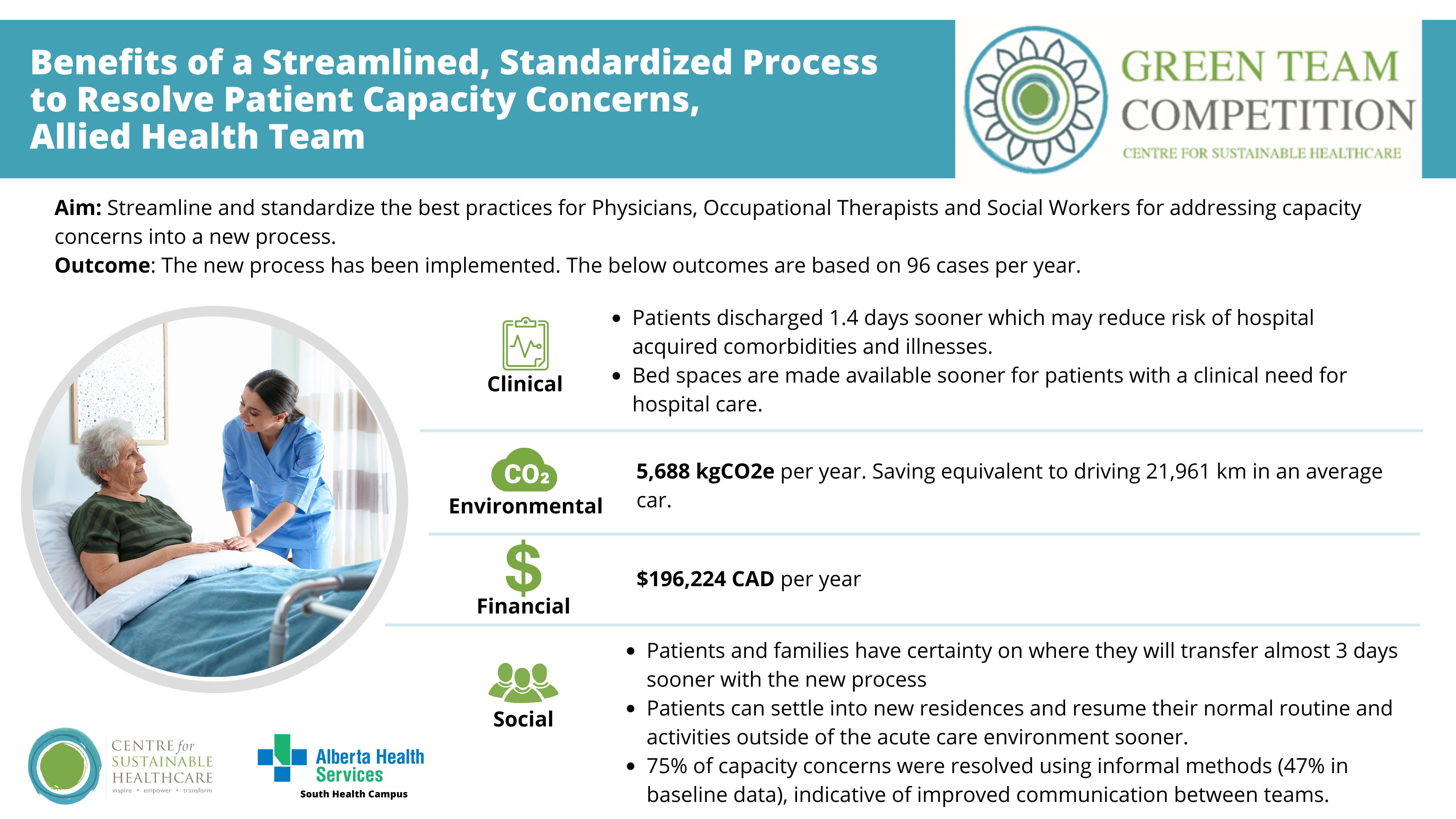
6. Triple bottom line: Benefits of a streamlined, standardised process to resolve patient capacity concerns, Allied Health
Team members: Sean Sloan, BSc, BScPT - Program Facilitator; Tracy Smith, BSW, MSW, RSW - Social Work Clinical Practice Leader; Shauna Thomas, BSc. O.T.(c), MClSc.W.H. - Occupational Therapist Clinical Practice Leader; Nancy Egbogah, RN, MN - Hospitalist Liaison Nurse; BSW, RSW - Inpatient Social Workers
Setting / patient group: Inpatient setting. Patients requiring pre-capacity assessment prior to discharge either to home or a disposition location.
Issue
The team identified that the pre-capacity assessment process and MDT (multidisciplinary team) collaboration could be optimised to improve patient care.
Intervention
The project aimed to streamline and standardise best practices for Physicians, Occupational Therapists, and Social Workers when addressing capacity concerns, resulting in a new process.
The team evaluated their current process and identified inconsistencies and barriers to find opportunities for improvement. Several changes were made, including standardising assessment orders and the use of SmartPhrase, developing a process for communicating results of pre-capacity assessments through electronic messaging, creating a workflow/decision tree that identified clear alternatives to formal pre-capacity assessments, and providing education to Physicians, OTs, and SWs regarding the importance of ongoing and regular communication to guide them through the pre-capacity assessment process.
Outcomes
Patient Outcomes:
- Patient capacity concerns were resolved using informal methods in 75% of cases in the project cohort compared to 43% of cases in the baseline sample.
- Pilot results show that patients were discharged 1.4 days sooner compared to baseline data.
- 75% of pre-capacity assessments had a new OT and SW order placed when the physician determined a pre-capacity assessment was required.
- Use of the SmartPhrase in pre-capacity orders improved to 75% (3 out of 4 cases) from a baseline of 31%.
Environmental Sustainability: Based on the change being applicable to 96 patients per year, 5,688 kgCO2e will be saved, equivalent to driving 22,000 km.
Economic Sustainability: Annual financial savings are estimated to be $196,224 CAD, attributed to the reallocation of beds to acute care patients.
Social Sustainability:
- Patients and Families: With the new process, patients and families had certainty on where they were going to transfer almost 3 days sooner. Patients were discharged 1.4 days faster, allowing them to settle into their new residences sooner and resume normal routines and activities outside of the acute care environment. A reduced length of stay may also decrease the risk of hospital-acquired comorbidities and illnesses.
- Staff: The project demonstrated that 75% of capacity concerns were resolved using informal methods, compared to 47% in baseline data. This is highly indicative of improved communication between the teams, leading to fewer inappropriate requests for formal pre-capacity assessments.
Key learning point
The success of this project was driven by strong engagement from our physician group, along with our Occupational Therapists and Social Workers. PDSA (Plan-Do-Study-Act) cycles enabled us to implement changes, then adjust our resources and education to support the team as we rolled out the new process.