Leeds Green Ward Competition anticipates an annual reduction of 8,594.8 kgCO2e
This year, five teams from Leeds Teaching Hospitals NHT Trust participated in the Green Ward Competition, a clinical leadership and engagement programme for NHS Trusts to improve their sustainability within their service.
Climate change has far-reaching impacts on global health. Whilst healthcare systems have a key part to play in maintaining health in the face of the threat of climate change, the delivery of healthcare is also undermining the health of our populations by contributing to the problem. If healthcare were a country, it would be the 5th largest carbon emitter in the world. It is estimated that the England health and care system accounts for 4-5% of the country's carbon footprint.
Leeds Teaching Hospitals have been taking great steps to achieve the NHS target of achieving net zero by 2040. Last year, they were the first NHS Hospital Trust to become officially Carbon Literate, they won the Sustainable Hospital and Innovation in Mental Health Awards, and their general and emergency surgery team won the Green Surgery Challenge with their innovative project that focused on using a gasless procedure for laparoscopic appendectomy.
The five teams who entered the Green Ward Competition received mentoring from the Centre for Sustainable Healthcare to develop, run and measure projects that add sustainable value within their service, by considering the ‘triple bottom line’ of reduced environmental harm, reduced financial waste, and adding social value.
At the 19th of May Judging and Awards Ceremony, the five teams presented their projects, including the anticipated savings and opportunities to scale and spread. The judging panel consisted of Daniel Barrett, Head of Sustainability and Net zero North and East Yorkshire, Greener NHS, Sophie Williams, Operational Improvement Specialist, and Catherine Floyd, Clinical Specialities Lead at the Centre for Sustainable Healthcare (CSH).
Team 1: The Gloves are off on the paediatric intensive care unit
The paediatric intensive care unit (PICU) team focused on reducing the use of non-indicated sterile gloves during preparation and administration of oral and enteral medications.
Their team identified when non-sterile gloves were being used unnecessarily through an audit and literature review, prior to launching an awareness and education campaign aimed at reducing nursing use of gloves during medication administration. They anticipate a 25 percent reduction in nursing glove use in PICU is feasible.
- Environmental outcomes: A 25% reduction would save between 2242.73 kgCO2e - 3997.19 kgCO2e per year (based on bed space occupancy from 11-18 patients).
- Financial outcomes: A reduction in use by 25% will save between £1965.81 - £3216.79 per year (based on bed space occupancy from 11-18 patients).
- Social outcomes: Positive attitudes from staff, and potential for reduced rates of workplace related contact dermatitis for staff.
- Clinical outcomes: Potential for improvement in hand hygiene and with this, a reduction in hospital acquired infections.
Team members: Grace Crossland - PICU Staff Nurse, Dr Jonathan Ince - Simulation Fellow, LTHT, Dr Alex Olney - ST3, Paediatrics
Team 2: A Greener ‘Hub’ - A more sustainable vision for Medical Education within the Undergraduate Hub
The education team aimed to reduce the impact of their self-directed practice (SDP) rooms by streamlining equipment packs for naso-gastric tube (NGT) insertion, arterial blood gases (ABG), Venepuncture, and Cannulation and Catheter skills (the 5 most practiced skills).
A baseline inventory and audit identified items that were:
- Not required (unnecessary to the student experience nor reflective of real-life clinical practice).
- Required and a) potentially reusable, b) single use (needs to be replaced and purchased each time).
- Damaging to expensive equipment (e.g., alcohol-based cleaning solutions damaging to material of training arms, reducing their life span).
- Missing from the packs, which would be beneficial for student experience (e.g., gauze).
Equipment packs were streamlined for the five most popular clinical skills. The new packs were collected from students upon their arrival and remade by staff at the conclusion of each week, with any single-use items (e.g., canula) being replaced. Equipment collection trolleys in the SDP rooms had repurposed boxes for students to place their equipment into when finished. At the end of each month, a running total of CO2e savings equivalent to miles driven in a car was displayed on a whiteboard in each SDP room.
- Environmental outcomes: The annual predicted savings amount to 538.1579 kgCO2e. The team has also applied for funding for tablet devices. The tablets will enable students to practice electronic prescribing, access clinical practice videos and help in the running of mock examinations, which could save the department 26,280 sheets and an additional 113.72KgC02e.
- Financial outcomes: The new packs will save the department £623.39 per year.
- Social sustainability: Engaging medical students in sustainable action sparked enthusiasm for sustainable medical education across the student cohort, management, and Postgraduate teams. It has led to further projects including action to embed sustainability into teaching.
- Clinical outcomes: Potential for wide impacts due to the number of students utilising SDP rooms. When asked whether students had changed their practice as a result, responses were encouraging, e.g. “After this, I will be more mindful of how much equipment I take out of their packets on the ward”.
Team members: Cleone Pardoe – Clinical Teaching Fellow, Post-IMT2 Doctor, Alexander Strother – Clinical Teaching Fellow, Post-FY2 Doctor, Linh Mao – Undergraduate Medical Education Clerical Officer & Receptionist, Amanda (Mandy) Shotton – Undergraduate Medical Education Service Manager
Team 3: Changing blood test postage kits for patients on the renal transplant register
Patients active on the transplant register and those listed for simultaneous kidney and pancreas transplant must have regular blood tests (every 1-3 months) to re-examine their antibodies. With patients all over the region, transporting these samples to the laboratory can be logistically challenging and expensive. The renal team aimed to measure the environmental, social and financial benefits of a new postal system compared with an old postal system.
Previously, patients would be sent a blood tube in a large “Safe lock” box which had to be sent back to the hospital from a post office, at an inconvenience to the patient. The boxes themselves were expensive and single use, creating a large amount of plastic waste. The use of a lightweight, recyclable plastic pouch with pre-paid postage labels has been implemented, eliminating the trip to the post office (in favour of the closest post box) to the convenience of patients.
- Environmental outcomes: The total emissions per test (kit + postage) were reduced by 5.495 kgCO2e, extrapolated across a year with 222 tests sent, this is a saving of 1219.9 kgCO2e.
- Financial outcomes: With a saving of £8.79 per kit, they will save £1951.38 per year.
- Social outcomes: New postage blood test kits are easier to use and more convenient to return. Organising and sending out the new tests via internal post has been easier and faster for staff in the renal transplant office.
- Clinical outcomes: No change to or negative impacts on patient care.
Team members: Natalie Bird - Clinical Nurse Specialist, Renal Transplant, Laura Kirk - Clinical Nurse Specialist, Renal Transplant, Jo Wales - Clinical Nurse Specialist, Live Renal Donation, Jo Hitchings - Senior Clinical Support Worker
Team 4: The patient environment access team supports clinical areas to be more sustainable
The patient environment access team (PEAT) aimed to engage and increase staff awareness on sustainable actions, and successfully implement active dry mix recycling (DMR) and battery recycling.
An audit revealed that only four of fifty-six areas were actively using dry-mix recycling (DMR), and 0/56 areas had battery recycling bins. For most areas, batteries were being placed in a Sharp Smart Waste container. To ensure the long-term viability and sustainability of the project, recycling bins for DMR and batteries were installed in PEAT-scheduled areas. Trial DMR bins were placed in clinical staff break rooms that did not face patients.
- Environmental outcomes: 811.4 kgCO2e (7000kgCO2e if scaled to remaining suitable areas).
- DMR: Waste disposal emissions were reduced by 9.47 kgCO2e for the 7 areas per week (492.89 kgCO2e per year). If applied to the remaining 79 areas (excluding 4 that already had DMR), the projected annual saving is 5562.62 kgCO2e.
- Battery bins: Emissions reduced by 1.25 kgCO2e on average per week, per trial area. Projected at 70%, the potential annual saving across the 7 trial areas would be 318.5 kgCO2e. As a conservative estimate, if we apply battery recycling across the remaining 76 areas in the trust with 30% applicability, an additional 1,482 kg CO2e could be saved across the Trust.
- Financial outcomes: £317.30 (£1652.70 if scaled to remaining suitable areas).
- DMR in the 7 trial areas saved the Trust approximately 50p per week, with an annual saving of £26.11. If applied to the other 79.00 areas with no DMR this would be a projected annual saving of £294.71.
- Battery recycling saved £1.15 on average per area per week. Projected at 70%, there is a potential annual saving of £291.20. Projected at a conservative 30% across remaining 76 areas £1,358 could be saved annually across the Trust.
- Social outcomes: Engagement with clinical teams showed that staff care about becoming more sustainable. The sustainability leaflet has supported awareness and so far, the sustainability team have received requests for DMR recycling in clinical areas.
- Clinical outcomes: No change to or negative impacts on patient care.
Team members: Jemma Robinson - Facilities Operational Manager, Carl Hyatt - PEAT Technician, Matthew Robinson - PEAT Technician, Claire Flanagan - Facilities Operational Manager, Project Support - Matthew Quinton - Waste Compliance and Sustainability Manager
Team 5: Review of the haemodialysis processes in a single satellite dialysis unit with the aim to reduce carbon, water and electricity waste
It is estimated that 3.8 tonnes of carbon-dioxide equivalent emissions are produced by one patient’s dialysis treatment per year. A single dialysis machine in the unit is routinely used for the provision of two dialysis treatments in a 24 hour period. However, dialysis machines are turned on at the beginning of the day, meaning dialysis fluid runs continuously whilst waiting for the patients to be connected. Each dialysis machine gets three heat disinfections per day. The team made changes to only turn machines on when a patient was connected and ready for their treatment, and to reduce the number of disinfections of the dialysis machines to once in 24 hrs, replacing the other disinfections with a rinsing process. The team also identified that they could reduce the number of pharmacy deliveries from weekly to biweekly to the satellite dialysis unit.
- Environmental outcomes: 1,914.4 kgCO2e per year. If implemented across the Leeds haemodialysis service, the estimated annual savings are 15,919.2kgCO2e.
- Financial outcomes: £2,837.05 (£33,435.30 if scaled to all Leeds dialysis units).
- Social outcomes: Changes support in reducing staff workload. Enthusiasm and interest from wider team will support ongoing work towards longer-term aims and in scaling changes to other dialysis units.
- Clinical outcomes: May contribute to improvement in patient turnaround, for example from saving time by replacement of disinfection (40 minutes) with rinse (9 minutes) of the machine in between patients.
Team members: Alison Hardy – Satellite Dialysis Unit Sister, Peter Jones – Renal Technical Services Manager, Terence Simpson – Renal Technologist, Dr V R Latha Gullapudi - Consultant Nephrologist, Dr Mark Wright- Consultant Nephrologist and Haemodialysis Lead
The Renal Transplant Department team was highly commended for their project, and the Haemodialysis Team received the winning prize of £500 to expand on their project or to be reinvested into a sustainability project in their area.
Libby Sutherland, Sustainability Manager at Leeds Teaching Hospitals NHS Trust said:
Really well done, all of the teams have put together fantastic projects and I've been absolutely astounded by some of the figures, they are quite frankly staggering, but it makes me optimistic for how we can work together across the organisation and really embed some of these principles into the various specialties across the organisation, so really well done and thank you for your input and time into the projects.
Rachel McLean, Green Ward Programme Manager said:
“It has been a pleasure to work with the Leeds teams for the duration of their Green Ward Competition. Each team has shown enthusiasm and dedication to their projects throughout and I hope they all feel very proud of their achievements. All teams have exciting plans to continue to embed sustainability into their services by scaling their current projects and embedding sustainable value into new ones. I am looking forward to seeing how their projects evolve in the future.”
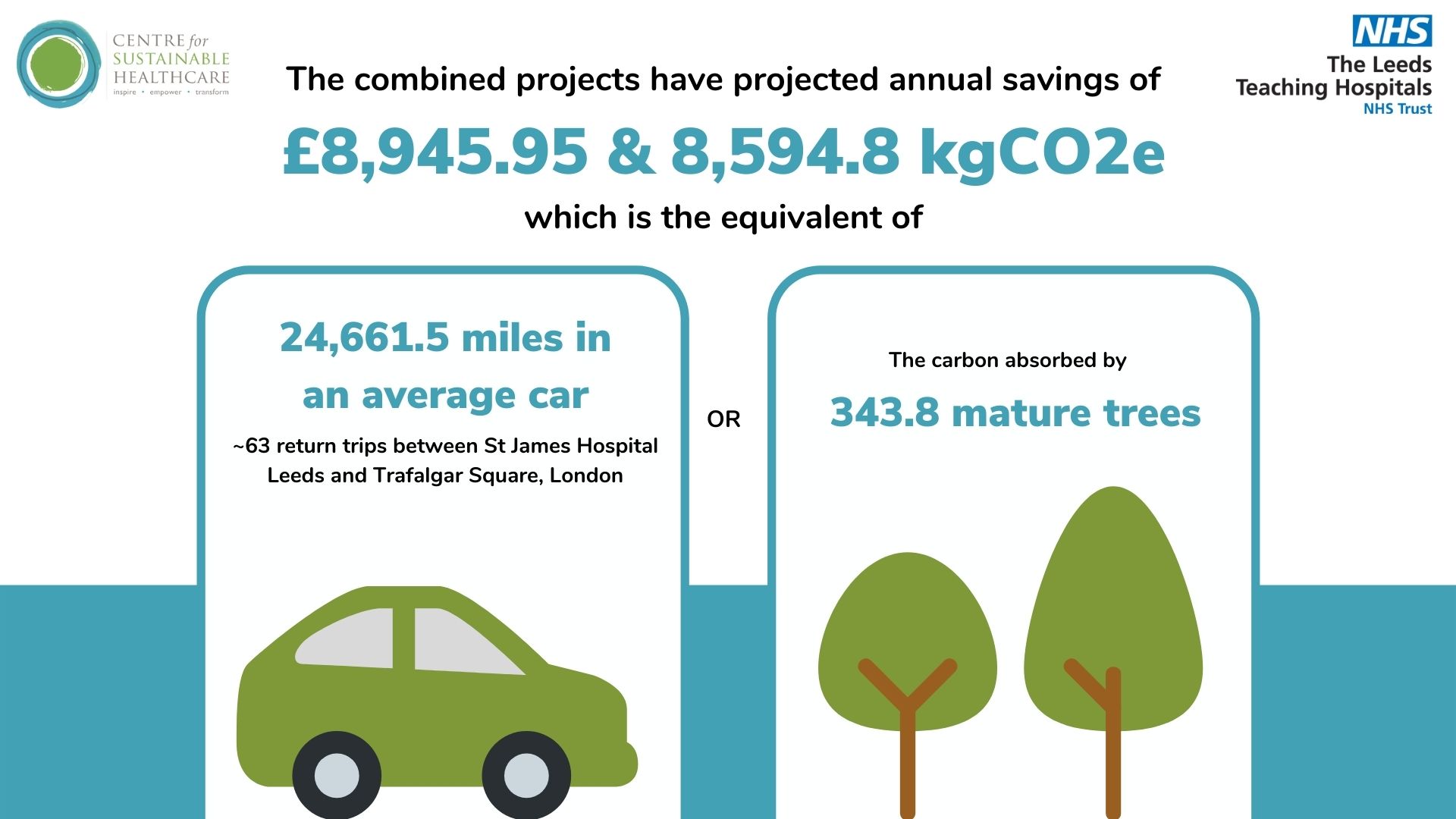
The combined projects of the five Green Ward Competition teams have projected annual savings of £8,945.95 and 8,594.8 kgCO2e, which is the equivalent of … The carbon absorbed by 343.8 mature trees in a year OR 24,661.5 miles in an average car (63 return trips between St James Hospital Leeds and Trafalgar Square, London)
With the potential to be scaled and spread further within their Trusts the teams have transformed their practice to be more environmentally sustainable, and have actively contributed to the NHS’s commitment to achieving net-zero by 2040.
If you are interested in running a Green Ward Competition at your organisation, please contact our Green Ward Program Manager Rachel McLean at rachel.mclean@sustainablehealthcare.org.uk for the most current pricing information.