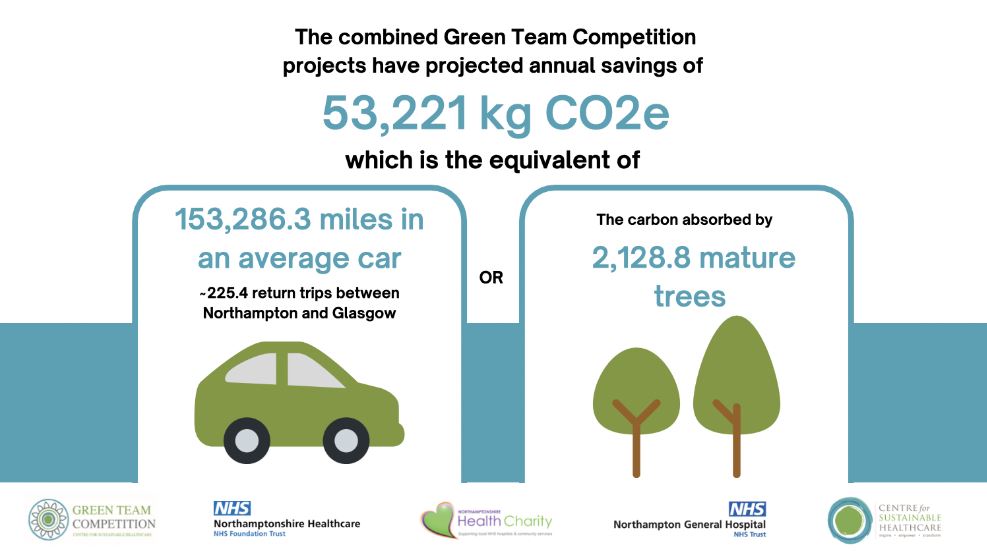
Northamptonshire Green Team Competition saves 53,221 kgC02e
Healthcare systems have a key part to play in maintaining health in the face of the threat of climate change, however delivery of healthcare is also undermining the health of our populations, by contributing to the problem. If healthcare were a country, it would be the 5th largest carbon emitter in the world.
The NHS was the first health service globally to commit to net zero carbon and was cited by the Intergovernmental Panel on Climate Change (IPCC) as a global leader. In the Delivering a Net Zero NHS report, strategies to achieve this target are laid out.
Running a Green Team Competition builds a community of clinical staff who are empowered, enthused, and equipped to further improve their services for the future and who actively transform healthcare by cutting carbon footprint, improving both patient care and staff experience while also saving money.
This year, Northamptonshire Health Charity made is possible for four teams from across Northamptonshire health services to engage in the Green Team Competition. The teams were supported by the Centre for Sustainable Healthcare to develop, run, and measure projects that add sustainable value to their service by considering the "triple bottom line".
At the October 21st Judging and Awards Ceremony, the four teams presented their projects, including the anticipated savings and opportunities to scale and spread. The judging panel consisted of:
- Paul Slater - Clinical Director Anaesthesia, Northamptonshire General Hospital NHS Trust
- Jean Knight - Chief Operating Officer, Northamptonshire Healthcare Foundation Trust
- Stuart Finn - Director of Estates and Facilities University Hospitals of Northamptonshire Group
- Keith Brooks - Director Northamptonshire Health Charity
- Cath Richards - SusQI Programme Lead, Centre for Sustainable Healthcare
The combined projects of the four Green Team Competition teams have projected annual savings of £71,529 and 53,221kgCO2e. Read the full Impact Report here.
Project summaries:
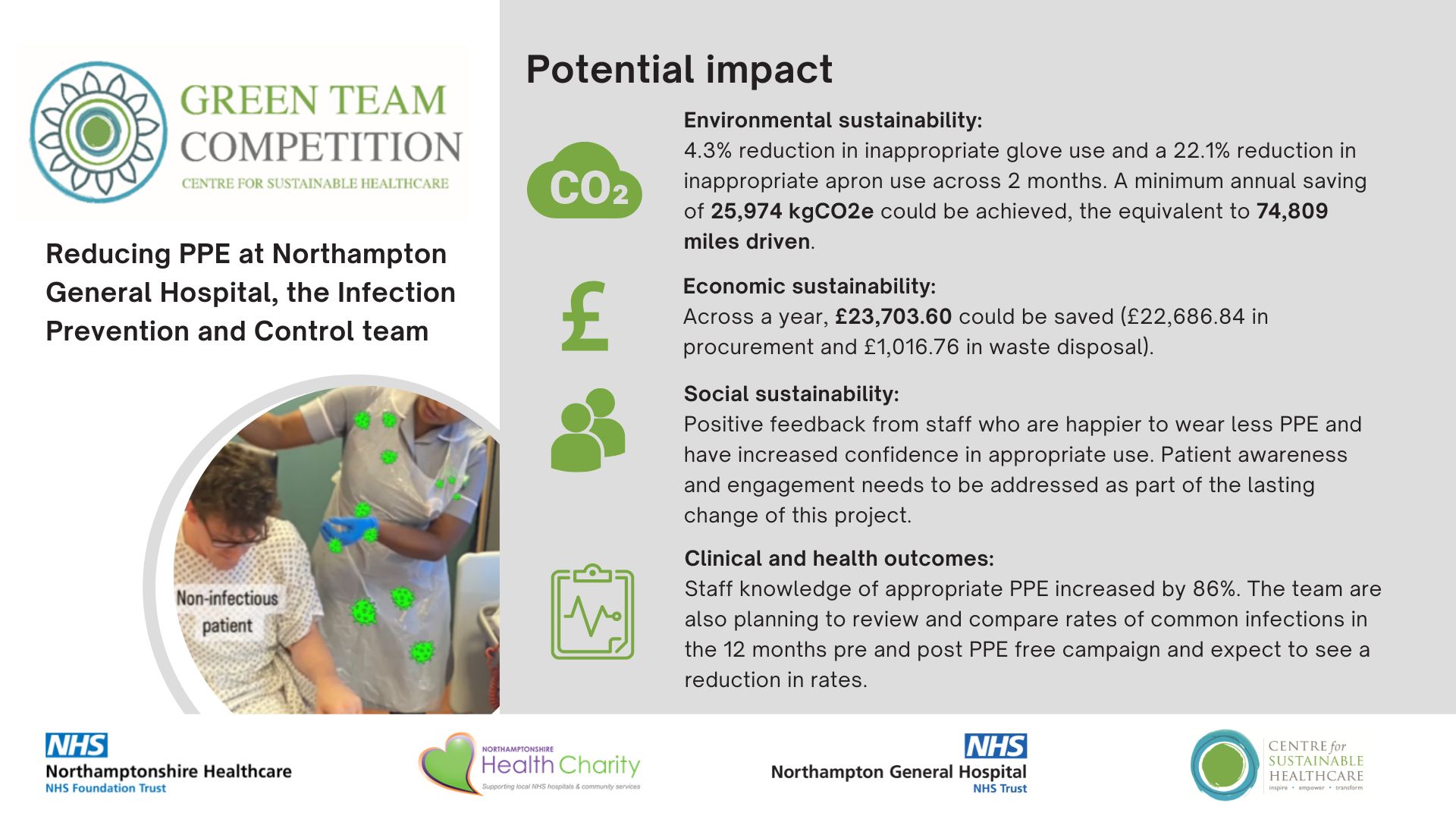
1. Greener Personal Protective Equipment: How the Infection Prevention and Control (IPC) team reduced PPE
Over 8.7 billion PPE items were distributed to health and social care services in England in 2021 compared to approximately 2.43 billion the year before. This pandemic-related increase in PPE has significant environmental, financial, and social implications.
The IPC team aimed to reduce inappropriate PPE use by 10% at Northampton General Hospital and increase staff knowledge of appropriate PPE use by 20% within the 10 weeks competition period.
Team members:
Project managers: Holly Slyne, Interim Director of IPC and Jasmine Lowdon Personal Protective Equipment (PPE) Coordinator; Video designer/editor: Risna Ferrer (IPC Nurse); Ros Pounds (IPC Matron), Meera Antony (IPC Nurse), Paul Scotland (Procurement Manager) and Rachel Pell (Head of Procurement).
Methods:
- The team reviewed current practice of PPE by:
- Observing usage on a surgical and medical ward.
- Testing PPE knowledge via a staff Facebook page quiz, asking them if they felt PPE was required for a specific task which would normally not require it.
- Reviewing their current PPE policy.
Using the observation and survey findings, 8 trends of PPE overuse were identified: wearing PPE to make a clean bed, to take patient’s observations, transporting patients, transferring patients, wearing the same PPE between patients, wearing to collect clean linen from the linen trolley, writing in patient notes and using the phone / computer at the nurse station
An education campaign was developed to reduce inappropriate PPE usage in clinical environments, with one theme targeted per week via:
- short educational videos posted on the staff’s Facebook page and on the wards’ WhatsApp groups.
- a screen saver with the theme on the staff’s intranet.
- posters placed throughout the trust.
- ward sisters and IPC team who educated staff on audits and huddles.
The PPE policy was updated and emailed out to ward managers asking them to educate their staff on when PPE is and isn’t required.
Results:
2. Critical Care getting ‘Pumped Up’ to reduce the unnecessary doses of PPI: a Critical Care team sustainable project focusing on patients’ welfare
Pharmaceuticals alone count for about 25% of carbon emissions in the NHS, the largest single contributing factor. The UK Governments 2021 National overprescribing review estimates 10% of medications dispensed in primary care are overprescribed. Literature has suggested that patients often continue taking proton pump inhibitor (PPI) medications for extended periods of time when no longer clinically indicated. This may be due to PPI being prescribed in an acute setting and continued through to and beyond discharge or prescribed in the community and dispensed on repeat.
Following this observation and with sustainability in mind, the Critical Care team aimed to reduce the number of unnecessary doses of PPI medications given to patients within critical care.
Team members:
Leeanne Hardy: Senior Sister, Quality Service and Improvement, Critical Care; Laura Moven: Junior Sister. Practice Education, Critical Care; Laura Robinson: Advanced Pharmacist for Critical Care; Rachel Kontogonis: Advanced Pharmacist for Critical Care.
Method:
The team reviewed their current practices by:
- Conducting a literature review into the relationships between PPI medication and poor health outcomes such as increased risk of CDI.
- Reviewing the indications and contraindications of PPI’s, using information from the Critical Care Compendium-Stress Ulcer Prophylaxis Guide
- Completing an audit of PPI prescriptions and administered doses for all elective patients to establish whether a PPI prescription or dose was necessary or not.
The team plan to deliver teaching sessions to both medical and nursing teams, expanding on the current ward checklists to include PPI reviews and increase awareness of an algorithm to aid review of patients admitted on PPIs.
Results:

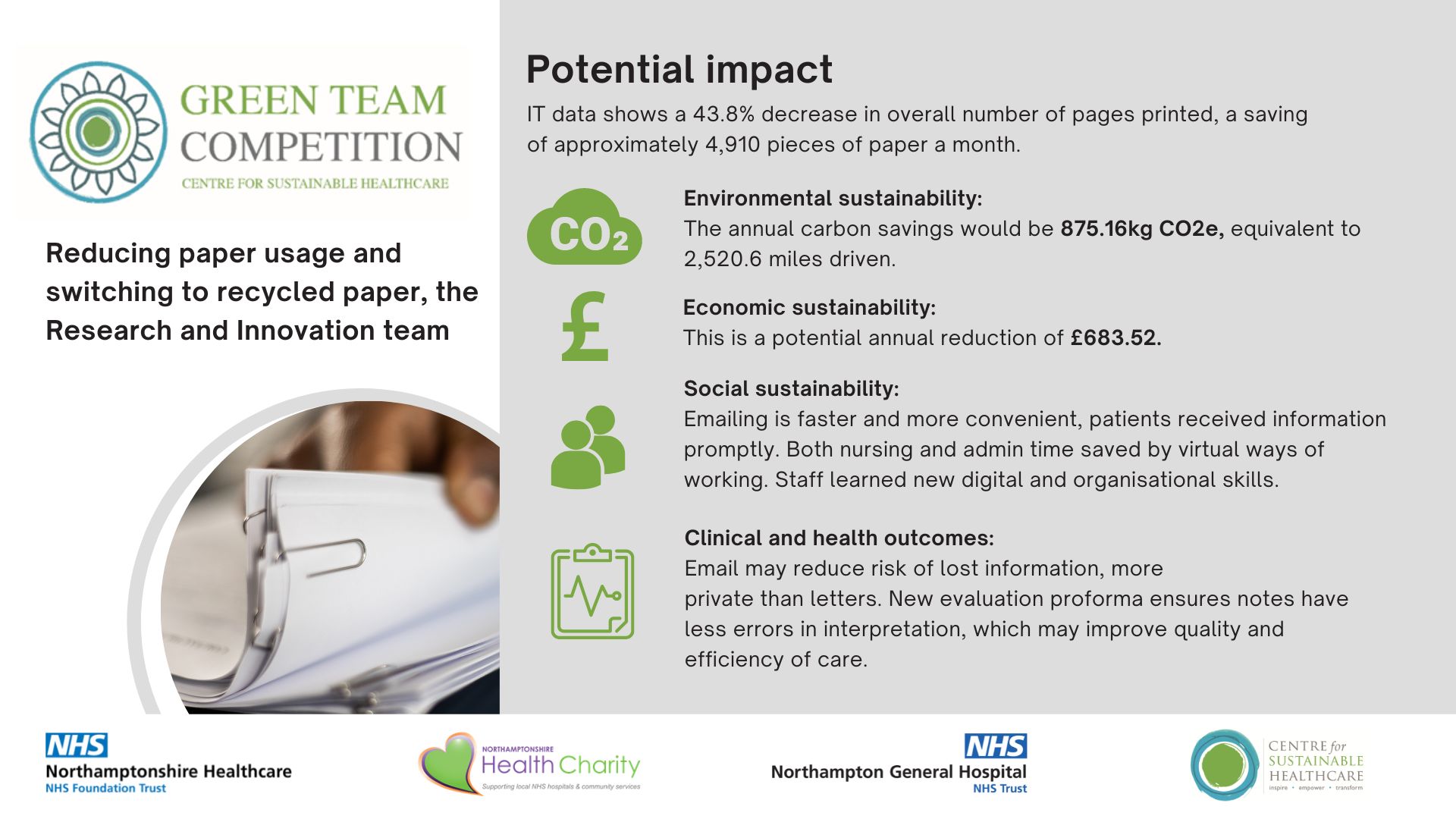
3. Reducing Paper Usage in the Research and Innovation department could help the Trust save £683.52 and 875.16kg CO2e annually
Research nurses facilitate research studies throughout the hospital. They help recruit patients to studies according to the individual study protocols and carry out trial treatments while maintaining patient safety. All studies have different sponsors and protocol requirements which means that direct changes to study visits and how they are conducted are difficult to implement, making it difficult to change patient care to improve sustainability. However, the Research and Innovation team identified that the tremendous amounts of paper they are using for these studies is as a carbon hotspot of their service: with approximately 45 studies open to recruitment and 39 studies in follow up currently, and each study may have between 2-10 large A4 folders full of paperwork.
Reducing paper usage by 50% and switching to 100% recycled paper by 2025 is one of the 13 key interventions set out in the Delivering a Net Zero NHS report to achieve a net zero NHS supply chain. The team aimed to significantly reduce their paper waste by diminishing their printing in the Research and Development service and effectively lower their carbon footprint.
Team members:
Andrea Kempa and Claire Woolhouse - Research Nurses
Method:
The team reviewed their current printing systems and team printing behaviours. They initially confirmed they were using 100% primary paper and quickly made a switch to 100% recycled paper.
Secondly, the team established a list of the varied reasons for printing in the R&I team and identified suitable changes that could be implemented to reduce printing in each area. To ensure staff engagement and a lasting shift in paper use practice they campaigned using several mediums:
- Emailed a short PowerPoint presentation to the team which included detailed data on their current paper use along with ideas for how to reduce this.
- Shared the NHS key printing principles from the Greener NHS How To Guide
- Placed a poster by both photocopiers to remind staff to “Think before we print” and only print what is necessary.
- Engaged in face-to-face mini ‘Green Workshops’ with their colleagues to personally reduce their printing based on their current printing preferences and behaviours.
- Trained staff in using digital tools to prevent excessive printing of protocols and manuals.
- An electronic nursing evaluation pro forma has been devised so that nursing notes can be typed up for patients whose notes are on MediViewer.
Results:
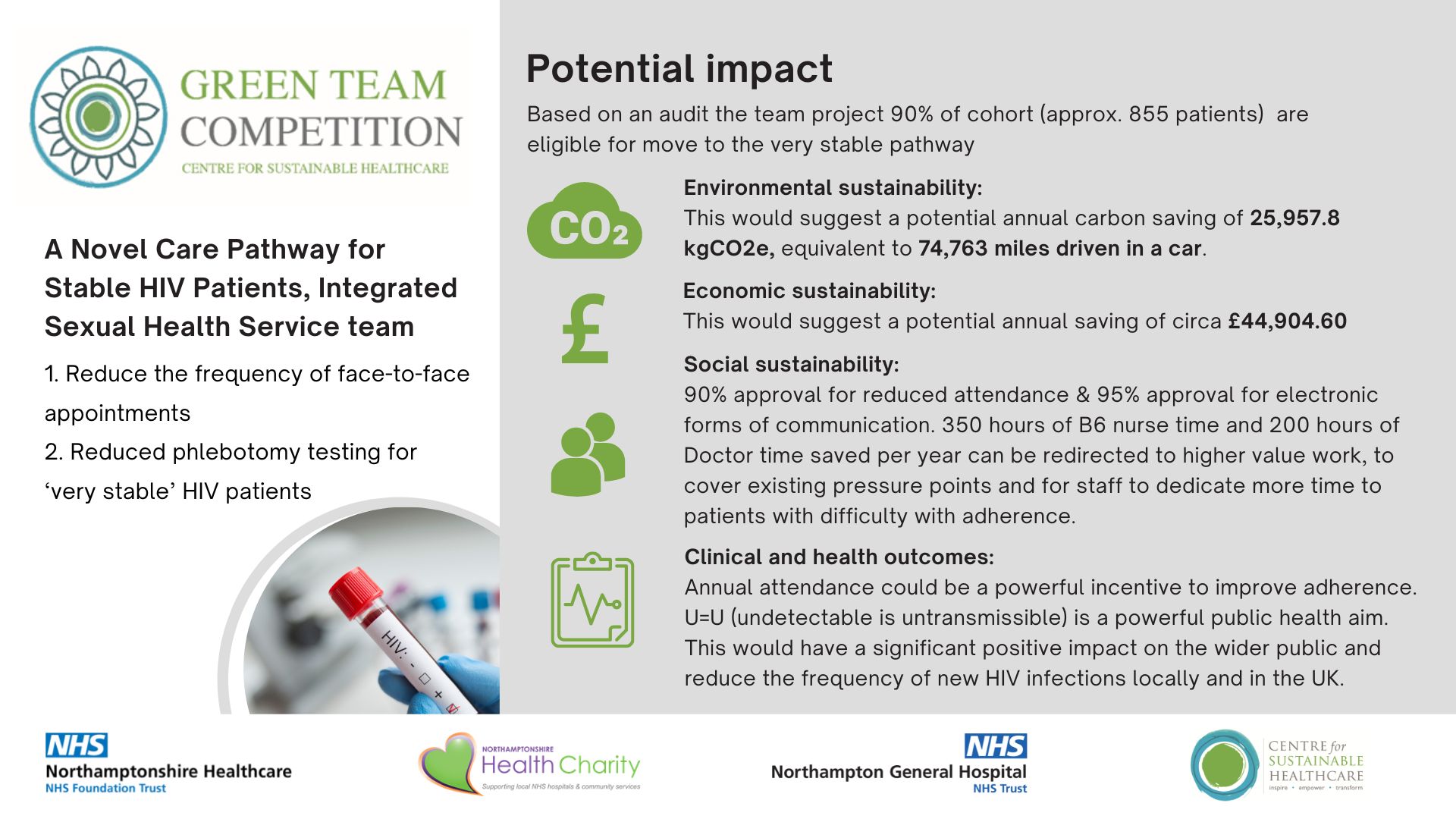
4. A Novel Care Pathway for Stable HIV Patients, presented by the Integrated sexual health service team
The increasing robustness and tolerability of antiretroviral treatment regimens for HIV over the last decade allows practitioners to consider the impact and necessity of multiple attendances by patients to hospital sites for pathology testing and examination. Most adherent patients are now physically stable, with personal and other employment commitments. Yet across the UK, most stable HIV patients attend NHS services with the same frequency and undergo the same/similar pathology investigations as those HIV patients who are relatively newly diagnosed or considered unstable.
Changing the clinical pathway for very stable patients to achieve a reduction in face-to-face appointments has the potential to provide environmental, financial, social and clinical benefits whilst maintaining patient confidence and safety.
For their Green Team Competition Project, the Integrated sexual health service team aimed to reduce the frequency of face-to-face appointments and phlebotomy testing for a defined ‘very stable’ section of the county HIV patient cohort in Northamptonshire from twice a year to once a year.
Team members:
Dr Lynn Riddell - Clinical Service Lead for Northamptonshire Integrated Sexual Health and HIV services (NISHH); Ms Eleanor Ingate - PA to Service Manager and Consultant Lead in NISHH; NISHH administrators, nurses, pharmacy and medical team.
Method:
The team reviewed their service and identified the existing minimum 6-month cyclical attendance pathway applies to all HIV patients, regardless of the stability of their condition and treatment. They proposed dividing the existing HIV cohort into three, as defined below;
- Cohort A / “Very Stable” patients: A definition of a “Very Stable” HIV patient was agreed between the county HIV consultants. Patient meeting the criteria will require annual attendance.
- Cohort B: Patients considered stable who still require more frequent (6 monthly) monitoring due to adherence issues or resistance to antiretroviral regimens requiring medication changes.
- Cohort C: Patients new to the service or newly diagnosed with HIV infection. They will have not commenced antiretrovirals or have commenced recently but their viral load is not yet undetectable. Cohort C will also include patients who are pregnant or clinically unwell with an HIV related illness. Cohort C will require frequent (sometimes monthly) monitoring with specific additional tests depending on their current issue.
All patients registered with the SU were notified of potential upcoming changes to their attendance schedule, and that the changes would be discussed with every patient at their next face to face appointment, and no patient would be moved to the annual pathway without their consent. At each patient’s next doctor appointment, a joint decision between the patient and the HIV doctor will be made as to whether this new pathway is suitable for the patient.
Results:
Awards
 Congratulations to the winning team, the Integrated Sexual Health Service team with their project ‘A novel care pathway for Stable HIV patients’, led by Dr. Lynn Riddell. The project challenged the team to question their service habits and ask, ‘why are we doing this?’, and, ‘who are we doing this for?’. The team kept the patient voice at the heart of their changes, and their resulting impacts are a great exemplification of the triple bottom line of sustainable value in practice. The Infection Prevention and Control team with their project ‘Be PPE Free!', received the highly commended award.
Congratulations to the winning team, the Integrated Sexual Health Service team with their project ‘A novel care pathway for Stable HIV patients’, led by Dr. Lynn Riddell. The project challenged the team to question their service habits and ask, ‘why are we doing this?’, and, ‘who are we doing this for?’. The team kept the patient voice at the heart of their changes, and their resulting impacts are a great exemplification of the triple bottom line of sustainable value in practice. The Infection Prevention and Control team with their project ‘Be PPE Free!', received the highly commended award.